Association of body weight and urinary tract infections during infancy: a nationwide comparative matched cohort study
Article information
Abstract
Purpose
This article was to investigate the association between urinary tract infections (UTIs) and high weight status in infancy.
Methods
We conducted a nationwide matched cohort study from January 2018 to December 2020 using data from the Korean National Health Insurance System and the Korean National Health Screening Program for Infants and Children. We analyzed the association between UTI diagnosis codes and high weight status (which was defined as being in the 90th percentile or higher of weight-for-age).
Results
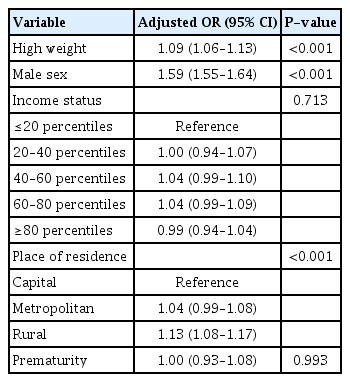
We found that 22.8% of infants with UTIs exhibited high weight status, compared to 20.0% of non-UTI infants (P<0.001). Per our multivariable analyses, the adjusted odds ratio for high weight status was 1.09 (95% confidence interval, 1.06–1.13).
Conclusions
UTI in the first 12 months of life was associated with a weight-for-age percentile of ≥90. Our findings corroborate those of previous single-center studies and emphasize the importance of careful monitoring for this at-risk group.
Introduction
Urinary tract infections (UTIs) are among the most prevalent bacterial infections in children [1], and their incidence stands at approximately 7.0% in febrile infants aged under 24 months [2]. Although UTIs have been considered to have a relatively benign course, potential complications such as kidney scars may develop. Kidney scarring, which occurs in approximately 15% of children following UTIs, can result in long-term severe consequences such as chronic kidney disease [3]. Consequently, conscious efforts to prevent UTIs and the accurate identification of their underlying risk factors are critical.
Infantile obesity, once considered benign and without significant concerns, has more recently been linked to childhood obesity; the body mass index (BMI) value of an infant is reported to be associated with their BMI value at the age of 5 years [4]. Considering the substantial role of adipose tissue in immune responses, deviations in adipose tissue quantities could potentially impact the immune system, resulting in increased susceptibility to infections [5]. Indeed, in the United States, an analysis of an inpatient database comprising subjects aged 2 to 20 years demonstrated a significantly increased risk of UTIs among obese females [6]. However, there is a paucity of specific data concentrating on the infantile period (during which UTIs are most prevalent). Two separate studies involving young children have been reported, both indicating an association between obesity and UTIs, although they were both single-center retrospective studies [7,8]. Infants may have prolonged contact with feces due to the lack of toilet training, leading to a higher incidence of ascending infantile UTIs. In addition to immune system alterations caused by adipose tissue, it is suspected that obese infants may have an abundance of internal bacteria in their perineal area due to its large contact surface, although this has not been confirmed by previous studies. In prior studies, a correlation was demonstrated between obesity and an increase in Escherichia coli within the gut microbiota, the most prevalent pathogen associated with UTIs [9,10]. Despite the existence of these predisposing factors, there is still a paucity of research specifically focusing on infantile UTIs and their association with body weight status. Recently, Yim et al. [11] conducted a nationwide cohort study to identify the association between body weight status and UTI development among children aged 4 to 71 months, in which they found that body weight status was associated with the development of UTIs among children aged 2 to 6 years.
In this nationwide population-based matched cohort study, we aimed to identify the association between body weight status and UTI during infancy, using data from the Korean National Health Information Database (NHID) and the Korean National Health Screening Program for Infants and Children (NHSPIC) data.
Methods
We conducted a nationwide population-based matched cohort study of Korean children born between January 1, 2017, and December 31, 2019, using NHID and NHSPIC data. Briefly, NHID data are provided by the Korean National Health Insurance System (NHIS), a Korean Ministry of Health and Welfare-affiliated mandatory healthcare system covering 99.4% of the 51 million people in South Korea. Korean NHSPIC is a health screening program for infants and children during well-baby check-up visits [12,13]. All children are eligible to participate in the NHSPIC seven times: i.e., at the ages of 4–6 months (1st), 9–12 months (2nd), 18–24 months (3rd), 30–36 months (4th), 42–48 months (5th), 54–60 months (6th), and 66–71 months (7th). Each program entails physical examination, anthropometric parameter (including height and weight) measurements, questionnaires, and anticipatory guidance for their age. The rate of participation in NHSPIC among all Korean children was 83.0% in 2020 [14], which implies that the results of NHSPIC can adequately represent the health status of Korean children.
Children eligible for this study were those who had claims data for UTIs at any time before reaching 12 months of age and who participated in the first NHSPIC examination between January 2018 and December 2020. UTIs were identified according to ICD-10 codes, which include acute pyelonephritis (APN) (N10), acute cystitis (N30.0, N30.8, N30.9, and B37.4), and unspecified UTI (N39.0 and P39.3). Controls were children who had visited the well-baby clinic and undergone the 1st NHSPIC examination without being diagnosed with UTIs. They were matched one-to-one with the study participants based on their birth year, birth month, and sex. Children with complex chronic conditions were excluded, derived from the Pediatric complex chronic conditions classification system version 2 [15].
Weight status, measured between 4 and 6 months of age, was dichotomized as at or above the 90th percentile and below the 90th percentile. We considered the following variables as covariates: sex, prematurity, parents’ socioeconomic status, and place of residence (categorized into capital, metropolitan, and rural). Data regarding income and area of residence were obtained from the NHIS qualification data, and information about prematurity was sourced from the 1st NHSPIC questionnaire. Categorical variables were presented as counts and percentages. We compared infants with UTI and those without UTI using a chi-square test. To investigate a potential association between high weight and UTI status, we performed a multivariable logistic regression analysis. We conducted two sensitivity analyses: first, we included the status of vesicoureteral reflux (VUR) and constipation as covariates (since they are known risk factors for UTIs) in sensitivity analysis model 1. Additionally, we excluded infants diagnosed with VUR from sensitivity analysis model 2. VUR was defined as having a diagnosis code of N13.7 or Q62.7, while constipation was defined as having a diagnosis code of K59.0. All statistical analyses were performed using R-project version 4.2.6 (R Foundation for Statistical Computing). The threshold for statistical significance was set at P<0.05.
Results
Baseline characteristics
A total of 153,453 children who experienced UTIs in infancy and received the 1st NHSPIC between January 1, 2018, and December 31, 2020, were enrolled. Among them, children with complex chronic conditions were excluded (n=17,927), leaving 135,526 infants affected by UTIs and 133,526 matched children not affected by them who were eligible for the main analysis (Fig. 1). Among them, 139,583 (51.9%) were boys and 3.88% (10,435) were born prematurely (Table 1).
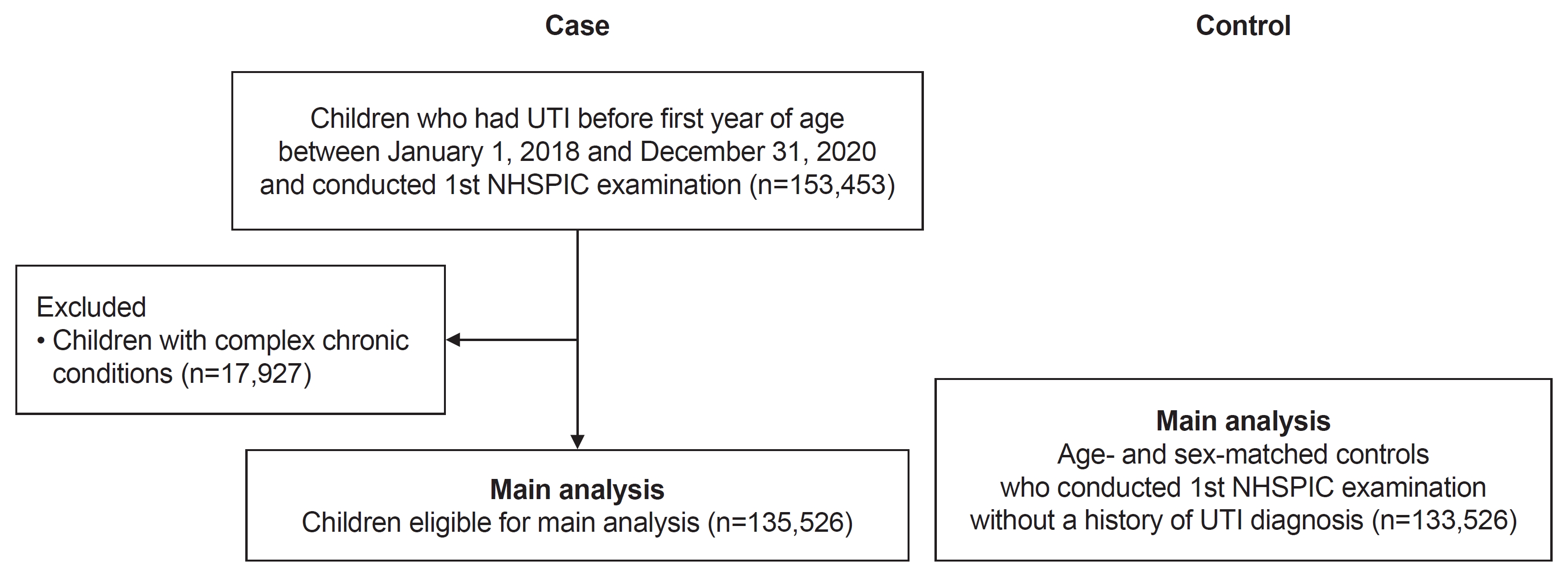
Flow diagram for study participants. UTI, urinary tract infection; NHSPIC, National Health Screening Program for Infants and Children.
Association between body weight status and UTI experience
Among infants with UTI experience, high weight (which was defined as weight-for-age ≥90th percentile) was significantly more prevalent than it was among infants without UTI experience (22.8% vs. 20.0%, P<0.001) (Table 1). Additionally, there were significant differences in sex, place of residence, and income status between those with UTI experience and those without it. Our multivariable logistic regression analysis revealed that high weight status remained significantly associated with UTI experience after adjusting for covariates, with an adjusted odds ratio (OR) of 1.09 (95% confidence interval [CI], 1.06–1.13) (Table 2).
Sensitivity analysis
The results of the multivariable analysis, which included VUR and constipation as covariates (model 1), and the analysis that excluded infants diagnosed with VUR (model 2), are shown in Table 3. Both sensitivity analyses demonstrated a statistically significant association between high weight and UTI experience after adjusting for covariates.
Discussion
In this study, we identified a statistically significant association between UTI occurrence during infancy and weight status. This association remained statistically significant even after adjusting for covariates and conducting various sensitivity analyses. The findings suggest that infants with a body weight-for-age above the 90th percentile may be more susceptible to infantile UTIs compared to those with weight-for-age values below the 90th percentile.
While congenital anomalies of the kidney and urinary tract, including VUR, are well-established risk factors for infantile UTIs, and circumcision and breastfeeding are well-known protective factors, a variety of environmental factors remain relatively underexplored. Various cross-sectional studies have identified obesity as a risk factor for UTIs in young children (encompassing children aged 2–6 years). However, research specifically focusing on infants aged below one year (who constitute the most susceptible group) is limited. Renko et al. [16] conducted a meta-analysis based on four studies, concluding that obesity predisposes to a higher risk of UTIs (OR, 2.23; 95% CI, 1.37–3.63), with two of them focusing on young children. Hsu et al. [7] reported that obesity was strongly associated with the presence of febrile UTI, and obese children (weight-for-age above the 95th percentile) aged 2 years or younger had a higher risk of developing a UTI than non-obese children (OR, 1.92; 95% CI, 1.15–3.21 in overweight [weight-for-age above the 85th percentile] children and OR, 2.46; 95% CI, 1.54–3.93 in obese children). Yang et al. [8] found that among children under 3 years, those classified as overweight or obese were significantly more predisposed to febrile UTIs (OR, 1.84; 95% CI, 1.11–3.05). However, both these studies were single-center studies. Recently, Yim et al. [11] reported that obesity in children less than 6 years of age were associated with subsequent UTIs during a 3-year follow-up period (hazard ratio, 1.13; 95% CI, 1.10–1.16), using the same platform of Korean NHID. However, obesity in children aged 4 months to 2 years did not show a clear association with subsequent UTIs (hazard ratio, 1.00; 95% CI, 0.97–1.03). In our paper, we conducted a cross-sectional comparison of weight status between infants with UTIs and non-UTI infants, and this yielded significant results [11].
Childhood obesity contributes to various pathophysiological changes, including heightened inflammation, altered adipokine signaling, metabolic shifts, and epigenetic modifications, all of which significantly impact immune response [17,18]. It is plausible to speculate that similar associations between weight status and UTI occurrence exist in young children for these reasons. However, direct measurements of associated changes in immunity have not been extensively investigated, which necessitates further research. Infants are generally more susceptible to ascending UTIs compared to older children. This vulnerability is attributed to factors such as a shorter urethra and a lack of toilet training. The absence of proper toileting increases the contact time between colonic bacteria and the urethral opening, which is a critical contributor to UTI development. In cases where obesity increases the surface area of contact between feces and skin within the diaper, the intensity of this contact is likely augmented. Previous studies have demonstrated an association between obesity and gut microbiota imbalance [9,10]. Gao et al. [9] revealed that obese children exhibit a higher abundance of E. coli compared to non-obese children. Additionally, an animal model study showed that the gut commensal E. coli exacerbates obesity and insulin resistance in mice [10]. Given that ascending UTIs are attributed to gut microbiota, the increase in E. coli within gut microbiota associated with obesity may exert more pronounced effects on infants. Nevertheless, these aspects remain relatively unexplored and necessitates further in-depth investigation and related studies.
A significant advantage of our study is the comprehensive, nationwide inclusion of children with UTIs. Given that the NHSPIC participation rate exceeded 80%, this study offers more reliability than investigations conducted at a single center. However, our study had some limitations. First, the categorization of the patient group was solely based on the diagnostic codes for APN, cystitis, and unspecified UTI, potentially leading to a detection bias. Second, due to limitations in our data source, we were unable to assess specific clinical manifestations like fever or severity such as the occurrence of urosepsis. These details would have been instrumental in the identification of any potential additional risks associated with high weight within these subgroups. Furthermore, given the limited power of our conclusion (adjusted OR, 1.09), the clinical significance of this finding would not be substantial, emphasizing the need for further research. Lastly, undetected covariates may influence the results due to the observational nature of the study.
In conclusion, UTIs occurring in the first 12 months of life were associated with a weight-for-age percentile of ≥90. This finding supports prior single-center study outcomes and indicates the need for meticulous monitoring of this vulnerable group.
Notes
Ethical statements
This study was reviewed and approved by the Public Institutional Review Board designated by the Korean Ministry of Health and Welfare (IRB No. P01-202207-01-029). The requirement for informed consent was waived because of the nature of the study.
Conflicts of interest
Ji Hyun Kim and Hee Gyung Kang are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, or decision process of this article. There are no other conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: YHA
Data curation: PGP
Formal analysis: PGP
Investigation: PGP
Methodology: YHA, HGK
Visualization: JHK
Writing-original draft: PGP
Writing-review & editing: YHA
All authors read and approved the final manuscript.