| Child Kidney Dis > Volume 27(2); 2023 > Article |
|
Abstract
Nutcracker syndrome (NCS) is a disease caused by compression of the left renal vein between the superior mesenteric artery and the abdominal aorta. Immunoglobulin A (IgA) nephropathy (IgAN) is characterized by the predominance of IgA deposits in the glomerular mesangial area. Hematuria and proteinuria can be present in both diseases, and some patients can be concurrently diagnosed with NCS and IgAN; however, a causal relationship between the two diseases has not yet been clarified. Here, we report two pediatric cases of NCS combined with IgAN. The first patient presenting with microscopic hematuria and proteinuria was diagnosed with NCS at the initial visit, and the second patient was later diagnosed with NCS when proteinuria worsened. Both patients were diagnosed with IgAN based on kidney biopsy findings and treated with angiotensin-converting enzyme inhibitors and immunosuppressants. A high index of suspicion and timely imaging or biopsy are essential for the proper management of NCS combined with glomerulopathy.
The nutcracker phenomenon (NCP), also known as left renal vein (LRV) entrapment, is defined as compression of the LRV between the superior mesenteric artery and abdominal aorta. Nutcracker syndrome (NCS) describes LRV entrapment with clinical manifestations, such as micro- to macroscopic hematuria, proteinuria, flank pain, abdominal pain, and varicocele [1]. Although the prevalence of NCS is unknown, it is increasingly being diagnosed owing to the development of diagnostic techniques [2,3]. Meanwhile, immunoglobulin A (IgA) nephropathy (IgAN) is the most common glomerulonephritis (GN) worldwide and leading cause of chronic kidney disease and end-stage kidney disease. Recurrent hematuria, with or without proteinuria, has also been reported in IgAN [4]. Although it is a rare presentation, several cases of coexisting NCS and IgAN have been reported [3,5-7]. In a Japanese study, the prevalence of NCP in 146 patients with IgAN was 6.8% [8]. Despite these reported cases, the relationship between these two diseases has not yet been clarified. Furthermore, it is difficult to diagnose and treat these patients appropriately. In this study, we report two pediatric cases of NCS combined with IgAN to suggest a relationship between the two diseases and emphasize their clinical significance.
An 11-year-old boy visited our hospital for the evaluation of proteinuria and microscopic hematuria, which were confirmed during a school health check-up. Two years prior, only microscopic hematuria was found during a school health check-up. The patient had no relevant family history. His body mass index (BMI) was 17.8 kg/m2 (25th percentile) and blood pressure was 113/76 mmHg (73rd percentile). Laboratory test results, including complete blood cell counts, electrolytes, and biochemistry tests, were unremarkable. Complement C3 and C4 levels were within the normal range; however, serum IgA level was elevated at 229 mg/dL (reference range: 53ŌĆō204 mg/dL). Results for anti-double-stranded DNA, antinuclear antibody, and antineutrophilic cytoplasmic antibody were negative. Urinalysis revealed 2+ protein and 5ŌĆō9 red blood cells/high-power field (RBCs/HPF). Random urinary protein-to-creatinine ratio (UPCR) in the early morning was 0.64, and protein amount in 24-hour urinalysis was 477 mg (14 mg/m2/hr). The protein measured in supine and erect positions for 12 hours was 157 mg (9.4 mg/m2/hr) and 193 mg (11.6 mg/m2/hr), respectively. Urine dysmorphic RBC testing was negative. On initial kidney Doppler ultrasonography, the blood flow velocity of the LRV at the renal hilum and aortomesenteric portion was 28.8 and 161.7 cm/s, respectively. The peak velocity ratio (PVR) was 5.61; therefore, the patient was diagnosed with NCS. He was treated with enalapril, and a kidney biopsy was performed due to worsened proteinuria with a UPCR of 0.70. Light microscopy revealed segmental glomerulosclerosis, tubular atrophy, and interstitial fibrosis (Ōēż25%) (Oxford classification: M1, E0, S1, T0, C0). IgA (3+), lambda (3+), kappa (2+), fibrinogen (2+), IgM (1+), and C3 (1+) levels in the mesangial regions were observed using immunofluorescence. Mesangial and paramesangial electron-dense deposits and focal foot process effacement (10%) were confirmed by electron microscopy. This result was consistent with IgAN. Deflazacort was initiated, but after 2 months, proteinuria was aggravated, with a 24-hour urine protein amount of 762 mg (23 mg/m2/hr). Subsequently, azathioprine was administered, and proteinuria and hematuria improved. Azathioprine and deflazacort were discontinued 2 and 4 years later, respectively, and the patient is now being treated with enalapril alone. Five years after the kidney biopsy, urinalysis showed a specific gravity of 1.04, 2+ protein, and 0ŌĆō1 RBCs/HPF. UPCR was 0.14, and protein levels in the 24-hour urine were 289 mg (7.62 mg/m2/hr). Proteinuria has been waxing and waning until recently. Based on recent laboratory findings, serum cystatin C level increased from 0.82 to 0.95 mg/L (0.53ŌĆō0.95 mg/L). Cystatin C-based estimated glomerular filtration rate was 99 mL/min/1.73 m2. Kidney Doppler ultrasonography was repeated, and NCS was confirmed (PVR, 6.37) (Fig. 1A-C). The patientŌĆÖs clinical course is shown in Fig. 1D.
A 7-year-old boy presented to our hospital with proteinuria and microscopic hematuria, which were confirmed during a school health check. His father had a history of thin glomerular basement membrane (GBM) disease, which was diagnosed during high school. His BMI was 16.4 kg/m2 (50th percentile) and his blood pressure was 101/64 mmHg (56th percentile). Laboratory test results, including complete blood cell count, electrolytes, and biochemistry tests, were unremarkable. Other blood examination results, including complement C3 and C4, IgA, anti-double-stranded DNA, antinuclear antibody, and antineutrophilic cytoplasmic antibody tests, were also normal. Urinalysis revealed 2+ protein and 30ŌĆō60 RBCs/HPF. The UPCR was 0.59, and protein amount in 24-hour urinalysis was 250 mg (11.3 mg/m2/hr). The percentage of dysmorphic urine RBCs in the specimen was 80%. The patient was treated with enalapril for the suspected GN. After 6 months, follow-up urinalysis revealed a UPCR of 0.17 and 10ŌĆō29 RBCs/HPF. The amount of protein in the 24-hour urinalysis was 98 mg (4.4 mg/m2/hr), and dysmorphic RBCs were not observed. Subsequently, enalapril was discontinued, and the patient was followed up. After 3 years, proteinuria with microscopic hematuria worsened. Urinalysis revealed 3+ protein and 30ŌĆō60 RBCs/HPF. The UPCR was 1.30, and the protein content in the 24-hour urine was 1,215 mg (34.4 mg/m2/hr). The patient was again treated with enalapril. A kidney biopsy could not be performed due to the parentsŌĆÖ reluctance. Kidney Doppler ultrasonography was performed. The blood flow velocity of the LRV at the renal hilum and aortomesenteric portion was 24.3 and 141.7 cm/s, respectively. The PVR was 5.83; therefore, the patient was diagnosed with NCS. Genetic testing for Alport syndrome using next-generation sequencing (CD151, COL4A3, COL4A4, COL4A5, COL4A6, FN1, MYH9, and PXDN) was negative. Despite maintaining enalapril, proteinuria with microscopic hematuria waxed and waned; therefore, deflazacort was initiated. Based on follow-up laboratory findings, the IgA level was continuously elevated at 232 mg/dL (53ŌĆō204 mg/dL). One year later, repeat kidney Doppler ultrasonography showed NCS, with the PVR increasing to 7.16. After deflazacort was initiated, proteinuria with microscopic hematuria improved, but proteinuria worsened after the patient and his parents decided to discontinue the medication (24-hour urine protein, 222ŌĆō757 mg/day). Cystatin C level increased from 0.93 to 1.07 mg/L (0.53ŌĆō0.95 mg/L) during the past year. Cystatin C-based estimated glomerular filtration rate was 86 mL/min/1.73 m2. Finally, his parents agreed for kidney biopsy, 5 years after the onset of the initial manifestations. Light microscopy revealed focal to diffuse mesangial proliferation and mild tubular atrophy. No glomeruli were globally sclerotic (Oxford classification: M1, E0, S0, T0, C0).IgA (3+), C3 (2+), kappa (2+ to 3+), lambda (3+), and fibrinogen (3+) levels in the mesangial regions were determined using immunofluorescence. Electron microscopy revealed an irregular contour and thickness of the GBM (115ŌĆō308 nm; mean, 197 nm) with multiple mesangial electron-dense deposits. IgAN was confirmed by renal biopsy (Fig. 2A-C). He is currently undergoing outpatient follow-up and maintaining enalapril and deflazacort therapy. The patientŌĆÖs clinical course is shown in Fig. 2D.
Herein, we report two cases of NCS combined with biopsy-proven IgAN in pediatric patients. Few studies have described the coexistence of NCS and IgAN with pathological and radiological confirmation, particularly in children. Cases of NCS combined with IgAN can occur and should not be overlooked because of the associated morbidity.
NCS can develop at any age, although mostly in the second and third decades of life [9]. The clinical manifestations of NCS include hematuria, orthostatic proteinuria, left flank pain, and, although rarely, pelvic congestion symptoms [1]. Hematuria and proteinuria are generally considered to be caused by elevated LRV pressure, resulting in the rupture of thin-walled collateral veins into the calyceal fornix [9]. NCS is diagnosed using various tools, such as kidney Doppler ultrasonography, computed tomography, magnetic resonance imaging, and retrograde left renal venography [2]. The first imaging tool for suspected NCS was kidney Doppler ultrasonography, with a sensitivity and specificity of 82.3% and 89% to 100%, respectively. However, there are no optimal cutoffs for PVR for diagnosing NCS in children due to the small LRV sampling area and measurement variability according to the patient positioning [10]. Park et al. [11] suggested that a cutoff value greater than 4.0 for the PVR should be used as a sonographic criterion to diagnose NCS in children. In our study, two patients were diagnosed with NCS through Doppler ultrasonography with a cutoff value greater than 4.0 for PVR. Meanwhile IgAN, characterized by predominant IgA deposits in glomerular mesangial areas, is the most common form of GN worldwide. Similar to NCS, the clinical features of IgAN can also present as macroscopic hematuria, asymptomatic microscopic hematuria with or without proteinuria, nephrotic syndrome, and, rarely, acute kidney injury [4]. Although the coexistence of NCS and IgAN is rare, several cases have been reported [3,5-8]; however, a clear correlation is yet to be confirmed. Ozono et al. [5] reported the case of two young adults with NCP complicated by IgAN. Compared to 10 patients showing only NCP, those with NCP and IgAN showed dysmorphic RBCs, suggesting glomerular hematuria, aggravation of hematuria after upper respiratory infections, persistence of proteinuria, urinary granular casts, and elevation of serum IgA levels. Subsequently, Shin et al. [3] reported a case of NCS combined with IgAN in a 9-year-old girl with gross hematuria. In a Japanese study [8], 10 of 146 patients with IgAN showed LRV entrapment, and all patients had dysmorphic urinary RBCs. Recently, a case of coexisting NCP and superior mesenteric artery syndrome in a patient with IgAN was reported [6]. In our study, the two boys were diagnosed with NCS and IgAN. Case 1 had a history of microscopic hematuria 2 years ago, and case 2 had a familial history of thin GBM disease. In case 1, serum IgA levels were elevated in the initial laboratory findings, and urine dysmorphic RBCs were not found. The serum IgA level in case 2 was initially normal but was continuously elevated during the follow-up examination, and dysmorphic RBCs were observed on urinalysis. While case 1 was diagnosed with NCS on initial kidney Doppler ultrasonography, kidney biopsy showed IgAN. In case 2, NCS was confirmed when proteinuria was aggravated 4 years after the initial presentation. The kidney biopsy findings were consistent with IgAN. A causal relationship between NCS and IgAN may exist because of their relatively common combinations.
Several studies have investigated how NCS can induce glomerular changes and are related to IgAN. According to the proposed hypothesis of the IgAN pathogenesis, increased amounts of galactose-deficient IgA1 are recognized as autoantigens by autoantibodies (mostly of the immunoglobulin G subclass) to form pathological immune complexes, some of which are deposited in the glomeruli and induce kidney injury [4]. Various pathological findings of IgAN are present in addition to IgA deposits in the mesangial areas on immunofluorescence. They are classified according to the Oxford classification as mesangial hypercellularity, endocapillary hypercellularity, segmental glomerulosclerosis, tubular atrophy/interstitial fibrosis, and cellular crescents [4]. In a study by Ha and Lee [12], kidney biopsy showed moderate mesangial hypercellularity and increased mesangial matrix in a patient diagnosed with NCS. These authors suggested that the mesangial lesions might have been induced by the angiotensin II (Ang II) effect caused by NCS. Keane and Raij [13] also found that the accumulation of phlogogenic macromolecules caused by Ang II in the glomerular mesangium may induce mesangial expansion and eventual glomerulosclerosis. Given that vascular endothelial cells actively participate both in innate and adaptive immune responses [14], LRV entrapment in NCS may cause venous congestion and endothelial activation, contributing to impairment of the immune system. Notably, in a recent large cohort study examining the association between NCP and GN, the prevalence of LRV entrapment was higher in patients with IgAN and IgA vasculitis with nephritis (Henoch-Sch├Čnlein purpura nephritis) after adjusting for age, sex, and BMI. Furthermore, glomerular IgA and galactose-deficient IgA1 deposition was more common in patients with lupus nephritis and IgAN-unrelated diseases with LRV entrapment than in those without LRV entrapment [7].
Kidney biopsy can be an important tool for the definite diagnosis of GN. In the present case, kidney biopsies were performed to diagnose possible combined GN. Since it is difficult to diagnose complicated IgAN in patients with NCS based on clinical and laboratory findings, kidney biopsy should be considered when proteinuria or hematuria is aggravated in patients with NCS. Conversely, kidney Doppler sonography can be performed in patients with an unusual clinical course of GN. While proteinuria with hematuria was initially reduced after immunosuppressant administration in case 1, proteinuria has since been waxing and waning and persisted for a long time relative to the kidney biopsy findings. As NCS persists, prolonged proteinuria can be attributed to both IgAN and NCS. In case 2, NCS was diagnosed when proteinuria was aggravated. Since he was not initially evaluated for the presence of NCS, we could not confirm how NCS contributed to the development and progression of IgAN. However, his proteinuria and hematuria were relatively severe in comparison to the kidney biopsy findings and persisted despite taking immunosuppressants. NCS continued on follow-up ultrasonography. Considering the mechanism by which NCS can influence glomerular changes mentioned earlier, NCS may have affected our patientsŌĆÖ disease courses. Furthermore, Shimada et al. [15] reported that renal congestion caused tubulointerstitial and glomerular injury in a rat model. In our cases, cystatin C levels were elevated, and considering the renal congestion associated with renal function decline, this observation can be attributed to NCS. Although additional studies are needed, our cases suggest that renal venous congestion due to LRV entrapment could induce proteinuria and hematuria, leading to renal damage.
Conservative care is the first-line treatment of NCS in children. In a systematic review, improvement or complete resolution was observed in nearly 95% of patients treated with a conservative approach over 24 months [10]. Compared with NCS, the clinical course of IgAN is variable, ranging from an asymptomatic non-progressive disease to a highly aggressive disease. Poor prognosis is correlated with proteinuria Ōēź1 g/day, sustained hypertension, and severe renal involvement. Angiotensin-converting enzyme inhibitors and Ang II receptor blockers can effectively control proteinuria and hypertension. Combined immunosuppressive therapy can be considered in patients with persistent proteinuria or worsened kidney function [4]. Since IgAN is a significant cause of chronic kidney disease, and NCS and IgAN have a different treatment and prognosis, it is important to diagnose these two diseases at an early stage and determine appropriate management to improve clinical prognosis in the future.
In summary, our studyŌĆÖs finding of NCS combined with IgAN may be coincidental; however, the relationship between the two disease entities is supported by our patientsŌĆÖ clinical courses and previous studies. Future multicenter studies involving large sample sizes are needed to clarify the relationship between NCS and GN, independent to IgAN. Despite NCS diagnosis, considering the presence of combined GN in case of aggravated proteinuria or hematuria is crucial for appropriate management. Furthermore, clinicians must be aware of combined NCS when the clinical course of GN is uncommon. Likewise, a high suspicion and timely imaging or biopsy are essential for the accurate diagnosis of NCS combined with glomerulopathy.
Notes
Ethical statements
This study was approved by the Institutional Review Board of Korea University Ansan Hospital (IRB No. 2023AS0135), and informed consent was waived due to the retrospective study design.
Conflicts of interest
Eujin Park and Hyung Eun Yim are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: HEY
Data curation: SHK, MHS, EP, HEY
Investigation: SHK
Methodology: SHK, MHS, EP, HEY
Project administration: HEY
Visualization: SHK
Writing-original draft: SHK
Writing-review & editing: SHK, MHS, EP, HEY
All authors have read and approved the final manuscript.
References
1. Granata A, Distefano G, Sturiale A, Figuera M, Foti PV, Palmucci S, et al. From nutcracker phenomenon to nutcracker syndrome: a pictorial review. Diagnostics (Basel) 2021;11:10.



2. Kolber MK, Cui Z, Chen CK, Habibollahi P, Kalva SP. Nutcracker syndrome: diagnosis and therapy. Cardiovasc Diagn Ther 2021;11:1140-9.



3. Shin JI, Park JM, Shin YH, Lee JS, Kim MJ, Jeong HJ. Nutcracker syndrome combined with IgA nephropathy in a child with recurrent hematuria. Pediatr Int 2006;48:324-6.


4. Rajasekaran A, Julian BA, Rizk DV. IgA nephropathy: an interesting autoimmune kidney disease. Am J Med Sci 2021;361:176-9.



5. Ozono Y, Harada T, Namie S, Ichinose H, Shimamine R, Nishimawa Y, et al. The ŌĆ£nutcrackerŌĆØ phenomenon in combination with IgA nephropathy. J Int Med Res 1995;23:126-31.



6. Wang C, Wang F, Zhao B, Xu L, Liu B, Guo Q, et al. Coexisting nutcracker phenomenon and superior mesenteric artery syndrome in a patient with IgA nephropathy: a case report. Medicine (Baltimore) 2021;100:e26611.



7. Wang F, Zhu H, Bao S, Qi H, Xu L, Liu X, et al. Associations of left renal vein entrapment with IgA nephropathy and Henoch-Sch├Čnlein purpura nephritis. Ren Fail 2022;44:1519-2.



8. Imai N, Shirai S, Shibagaki Y, Kimura K. Nutcracker phenomenon in IgA nephropathy. Clin Kidney J 2014;7:325-6.



10. Meyer J, Rother U, Stehr M, Meyer A. Nutcracker syndrome in children: appearance, diagnostics, and treatment: a systematic review. J Pediatr Surg 2022;57:716-22.


11. Park SJ, Lim JW, Cho BS, Yoon TY, Oh JH. Nutcracker syndrome in children with orthostatic proteinuria: diagnosis on the basis of Doppler sonography. J Ultrasound Med 2002;21:39-45.


12. Ha TS, Lee EJ. ACE inhibition can improve orthostatic proteinuria associated with nutcracker syndrome. Pediatr Nephrol 2006;21:1765-8.



13. Keane WF, Raij L. Relationship among altered glomerular barrier permselectivity, angiotensin II, and mesangial uptake of macromolecules. Lab Invest 1985;52:599-604.

Fig.┬Ā1.
Renal Doppler ultrasound and clinical course of case 1. (A) Left renal vein (LRV) entrapment between the abdominal aorta and superior mesenteric artery (SMA). (B) Peak velocity at the renal hilum, 23.5 cm/s. (C) Peak velocity at the aortomesenteric portion, 149.8 cm/s. (D) Follow-up 24-hour urine protein and peak velocity ratio (PVR).
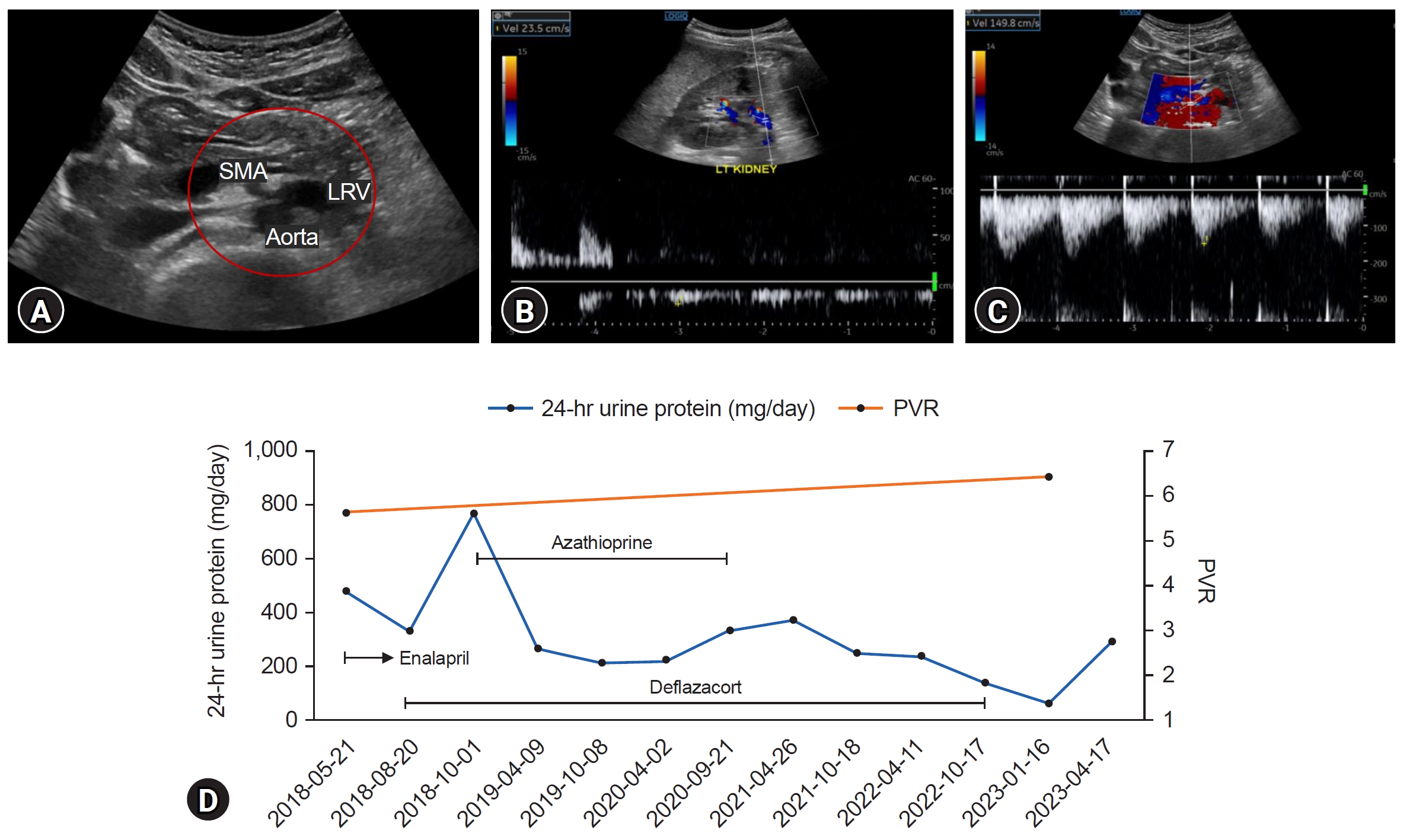
Fig.┬Ā2.
Renal biopsy findings and clinical course of case 2. (A) A glomerulus with focal to diffuse mesangial proliferation (black arrows) (periodic acid-Schiff stain, ├Ś400). (B) Strong immunoglobulin A (IgA) staining in mesangial regions (├Ś400). (C) Electron-dense deposits in the mesangium (black arrow) (├Ś4,000). (D) Follow-up 24-hour urine protein and peak velocity ratio (PVR).

- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 720 View
- 6 Download
- ORCID iDs
-
So Hyun Ki

https://orcid.org/0009-0003-0359-9231Min Hwa Son

https://orcid.org/0000-0002-4185-1712Eujin Park

https://orcid.org/0000-0002-4413-468XHyung Eun Yim

https://orcid.org/0000-0001-9805-9278 - Related articles




