A case report of tubulointerstitial nephritis and uveitis syndrome in children with an unfavorable outcome
Article information
Abstract
Tubulointerstitial nephritis and uveitis (TINU) syndrome is defined as the occurrence of tubulointerstitial nephritis and uveitis in the absence of other systemic diseases. Three pediatric cases have been reported in the Republic of Korea, and we now report a fourth case. A 15-year-old girl presented to the ophthalmology department with a 1-week history of bilateral ocular discomfort that worsened on the day of presentation with redness and pain in both eyes. She was diagnosed with bilateral uveitis, and her baseline examination revealed moderate renal dysfunction and mild proteinuria. A renal biopsy was performed and confirmed the diagnosis of TINU syndrome. She was started on steroid eye drops and a 12-week course of oral steroids at a dose of 40 mg/m2/day, which completely resolved the proteinuria and mild renal function to an estimated glomerular filtration rate of 60 mL/min/1.73 m2. However, the uveitis did not improve, and despite the addition of oral methotrexate as a second-line treatment, the uveitis remains unresponsive to treatment over 21 months. Further evaluation and treatment are ongoing, and active therapeutic intervention is suggested even at a pediatric age, considering the lack of improvement in renal function and uveitis to date.
Introduction
Tubulointerstitial nephritis and uveitis (TINU) is a rare disease that was first described in 1975 by Dobrin et al. [1]. It is characterized by a combination of decreased tubular function and uveitis, with reported incidences ranging from <0.1% to 2% across all age groups in uveitis centers [2]. The syndrome is known to have a higher incidence in younger age groups and in females. The pathogenesis of TINU syndrome involves certain genetic susceptibilities, medications, and infections as known risk factors. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) [3], antibiotics, and proton pump inhibitors have been identified as risk factors, and infections such as hantavirus, cytomegalovirus, Epstein-Barr virus, polyoma virus, adenovirus, human immunodeficiency virus (HIV), toxoplasmosis, varicella zoster, and tuberculosis have also been associated with the syndrome [2]. In addition, systemic immune disorders such as juvenile rheumatoid arthritis should be excluded in the diagnosis of TINU syndrome [4]. The disease is thought to have an immunologic basis, but a definitive pathogenesis has not been identified and genetic predisposition may play a role. Specific human leukocyte antigen (HLA) haplotypes, such as DRB1, DQA1, and DQA1, were statistically more prevalent among the TINU cohort than in an apparently healthy reference population [5]. Tubulointerstitial nephritis generally has a favorable prognosis, it often resolves without specific treatment, especially in children [6-8]. Our patient's renal function did not completely return to normal despite steroid treatment, and the uveitis did not respond to treatment at all despite the use of cytotoxic drugs.
Case report
The 15-year-old girl presented with a sudden onset of ocular redness, pain, and blurred vision in both eyes. She had a 1-week history of gradually worsening redness, pain, and blurred vision, accompanied by increased sensitivity to light and tearing. There was no previous history of similar symptoms and no recent ocular trauma or infection. Her past medical history was unremarkable, and she was not taking any medications at the time of presentation.
In an ophthalmic examination, her visual acuity was 20/40 in the right eye and 20/30 in the left eye (normal visual acuity; 20/20=1.0). Slit lamp examination revealed bilateral conjunctival injection, keratic precipitates, and cells in the anterior chamber. Fundus examination revealed uveitis and multiple scattered chorioretinal lesions in both eyes. Intraocular pressure was within normal limits in both eyes (Fig. 1). Based on these clinical findings, the patient was diagnosed with uveitis, specifically bilateral anterior uveitis with chorioretinal lesions. Further evaluation was performed to determine the underlying cause of the uveitis and to evaluate for associated systemic involvement. The patient was referred to a pediatric nephrologist for further evaluation and management of renal dysfunction. She was started on prednisolone eye drops for uveitis and antibiotic eye drops to prevent secondary infection. At the time of admission to the Department of Pediatrics, her height was 165 cm and her weight was 62 kg. A weight loss of 1 kg in 1 week was noted. Blood pressure was 110/60 mmHg. Her general condition was not so bad. No hematuria or edema was noted on history and physical examination. The urine output was more than 1,000 mL/day and the balance between input and output was good. Laboratory tests were normal results except for renal function. Specifically, her hemoglobin level was 9.5 g/dL, which was a little bit low for her age. Serum ferritin was 60.7 ng/mL. Hematocrit was 30%, platelet count was 323,000/μL, and white blood cell count was 6,400/μL with differential percentages of neutrophils (64.1%), lymphocytes (25.6%), monocytes (6.7%), and eosinophils (3.1%). C-reactive protein was 0.5 mg/dL, calcium/phosphorus ratio was 1.29 (9.8/7.6 mg/dL), aspartate aminotransferase and alanine aminotransferase were 32 and 34 IU/L, lactate dehydrogenase was 230 IU/L, and total bilirubin was 0.8 mg/dL. Serum levels of protein and albumin were 7.79 and 4.26 g/dL. Serum cholesterol was 126 mg/dL. Serum sodium was 140 mmol/L, potassium was 4.29 mmol/L, and chloride was 104.7 mmol/L. Urinalysis revealed 6 to 10 red blood cells per high-power field, urine protein-to-creatinine ratio was 0.31 (mg/mg), and fractional excretion of sodium was 1.08%. Urine calcium to creatinine ratio was 1.5 (mg/mg) and 24-hour proteinuria was 356.4 mg/day. Renal ultrasound findings were non-specific, and the right and left kidney sizes were 10.5 and 11.2 cm, respectively. Serum creatinine was elevated at 1.57 mg/dL, and the estimated glomerular filtration rate (eGFR; by bed side Schwartz Equations) was 43 mL/min/1.73 m2, confirming decreased renal function.
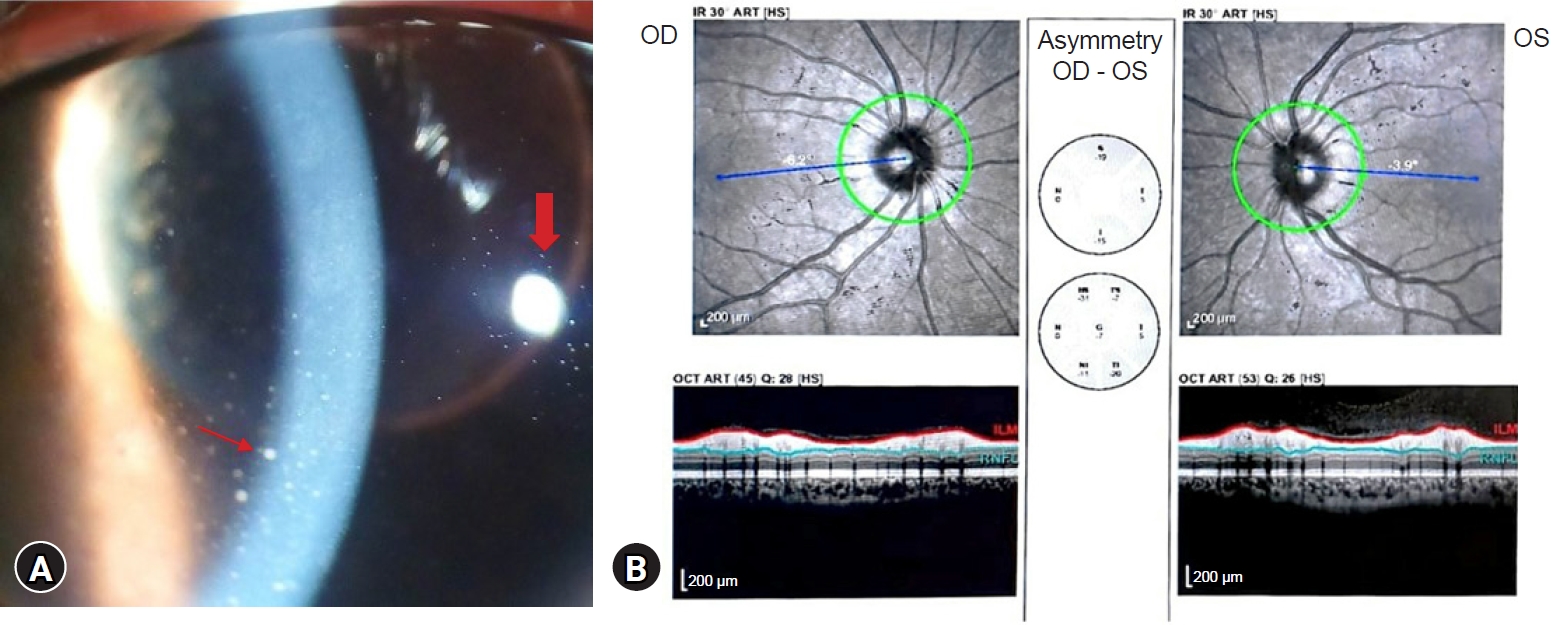
(A) Cells and keratic precipitates on the corneal endothelium and white blood cells and flare in the anterior chamber. The thin red arrow indicates leucocytes and flare. Thick red arrow indicates keratic precipitates on the corneal endothelium. (B) Optical coherence tomography shows asymmetry of both eyes, which was caused by nerve fiber edema extending toward the fovea in the left eye and venous turgor in the left eye.
OD, right eye; OS, left eye.
Additionally, serum herpes simplex virus immunoglobulin (Ig)M was positive, while venereal disease research laboratories test, anti-HIV, Epstein-Barr virus IgM, varicella zoster virus IgM, toxoplasma IgM, rubella IgM, cytomegalovirus IgM, and Toxocara canis IgM were all negative. Serum levels of complement (C)3 and C4 were 126 and 31 mg/dL. CH50 was 63.5 U/mL. IgG, IgA, IgM, IgE, and IgD levels were 1,740, 243, 217, 60, and 3.6 mg/dL, respectively. Autoantibodies, including antinuclear and anti-cytoplasmic antibodies, were all negative. HLA-B27 was also negative. A kidney biopsy was performed, which showed normal glomeruli and blood vessels, but with infiltration of inflammatory cells such as lymphocytes and plasma cells in the interstitium, and atrophied tubules, confirming the diagnosis of tubulointerstitial nephritis (Figs. 2, 3). The patient was initially treated with topical corticosteroid eye drops for uveitis and oral corticosteroids (40 mg/m2/day) for interstitial nephritis as initial treatment. Close monitoring was performed by both the ophthalmology and nephrology teams. Over the course of several weeks, the proteinuria gradually resolved and renal function improved, as evidenced by repeat laboratory tests showing complete resolution of proteinuria and a significant decrease in serum creatinine levels (1.13 mg/dL), although not yet fully normalized. However, there was no response to treatment for the presence of keratic precipitates or aggregates of cells in the anterior chamber. Nerve fiber edema and venous turgor did not improve. Subsequently, oral methotrexate of 10 mg was added to the treatment regimen due to the poor course of the uveitis, and the patient continued to be monitored and treated. Over the course of a year, the uveitis did not go into remission, so we increased the methotrexate to 15 mg. However, 21 months after the onset of uveitis, the disease persists in a similar manner (Fig. 4).
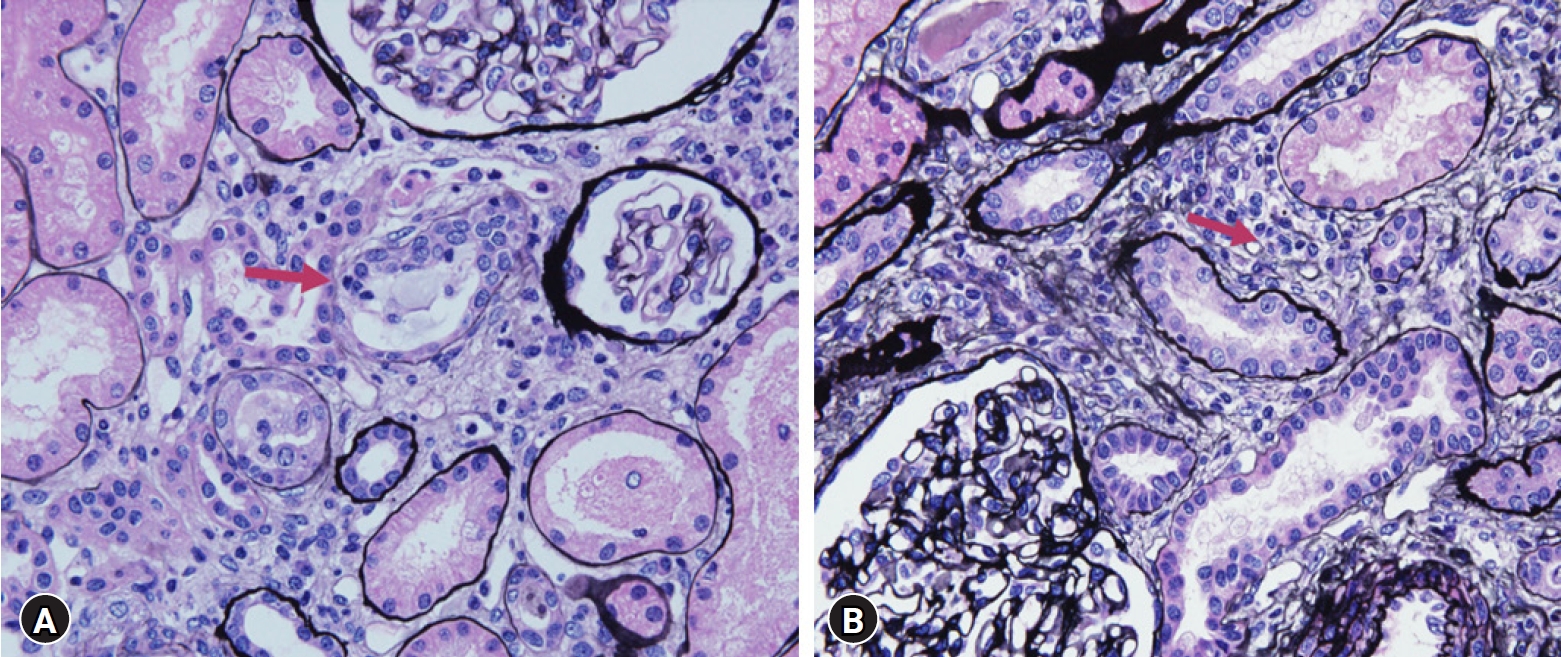
Pathologic findings. (A) Glomeruli and blood vessels were found to be normal, and the interstitium was infiltrated with inflammatory cells such as lymphocytes and plasma cells, and the tubules were found to be atrophied (silver stain, ×400). Red arrows indicate atrophied tubules. (B) Plasma cells and other types of inflammatory cells are seen in the renal tubules, and the tubules are atrophied. Red arrows indicate lymphocyte infiltration of the interstitium (silver stain, ×400).
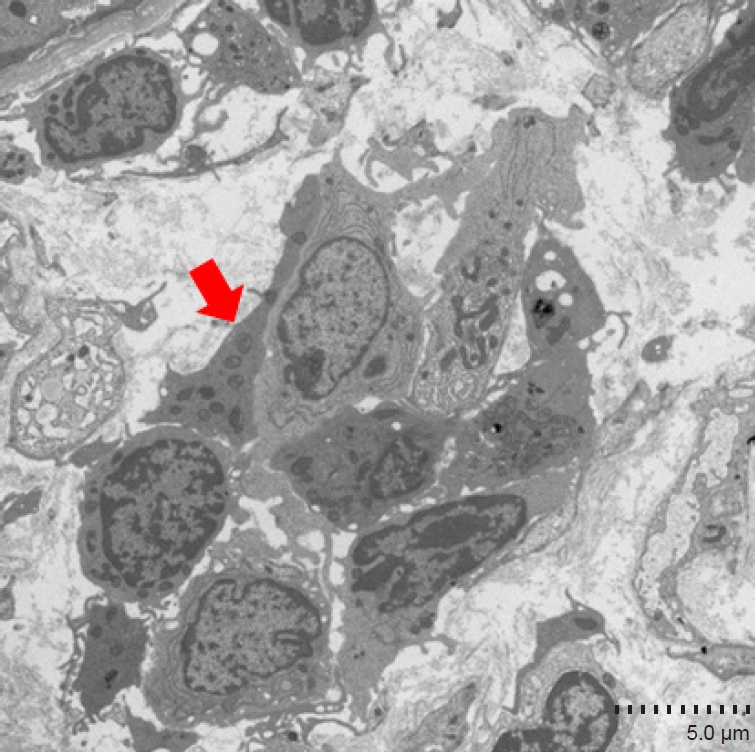
Electron microscopy reveals inflammatory cells in the tubules and fibrosis of the interstitium. The red arrow indicates inflammatory cells in the tubules.

Clinical course of patient over 1 year, proteinuria (A), serum creatinine (B), and eGFR (C) were significantly improved. Oral prednisolone (40 mg/kg/day) was prescribed for 12 weeks and the methotrexate of 10 mg was used. After 1 year, the dose of methotrexate was increased to 15 mg per day. Topical steroid for uveitis was used all the time. eGFR, estimated glomerular filtration rate.
Discussion
TINU syndrome is a rare and often underdiagnosed disease that presents with a combination of uveitis and tubulointerstitial nephritis. Three cases of TINU syndrome in children have been reported in Korea. Hahn et al. [9] reported a case of TINU in a 14-year-old girl. The acute interstitial nephritis resolved spontaneously, and the uveitis was treated with corticosteroid eye drops. Follow-up was conducted for more than 11 months. The authors noted that children often show spontaneous improvement and respond well to steroid treatment, whereas adults do not show as much spontaneous improvement in renal function. Therefore, the decision of whether to wait and see or start treatment, as done in children, is important in adults.
Kim et al. [10] reported a case of a 12-year-old boy who was successfully treated with systemic steroids and azathioprine. The treatment regimen included systemic corticosteroids (initially prednisolone, 2 mg/kg, and later deflazacort 1 mg/kg) and topical steroid drops for 1 month. Azathioprine was later added, and the systemic steroid was slowly tapered. The final outcome of the patient's TINU was favorable.
Lee et al. [11] described a case of a 9-year-old boy who was diagnosed with acute tubulointerstitial nephritis. After 2 months of treatment with prednisolone, renal function was normalized. However, anterior uveitis developed while tapering prednisolone and did not respond to systemic steroids but improved with cyclosporine. The patient presented with severe immunologic dysregulation, such as decreased peripheral CD3+, CD4+, CD8+ lymphocytes, reversed CD4+/CD8+ ratio, increased B lymphocytes, increased natural killer cells, polyclonal hypergammaglobulinemia, and various autoantibodies. The authors suggest that lymphocyte phenotypes and autoantibodies may provide more insight into the pathophysiology and clinical course of uveitis in TINU syndrome.
Pediatric TINU syndrome has a higher incidence than in adults, and it is important to consider TINU syndrome in the differential diagnosis of uveitis in children, even in the absence of systemic symptoms or history of medication use. In our case, the patient had no significant medical history, family history, or exposure to medications commonly associated with TINU syndrome, such as NSAIDs, antibiotics, or proton pump inhibitors. It has been suggested by researchers that TINU syndrome may have an immunological basis, as reported by Lee et al. [11]. However, we have not performed such detailed immunologic testing. A persistent immunologic derangement may be the reason for the chronic relapsing uveitis. Our patient was IgM positive for herpes simplex virus, but there was no clinical evidence of herpes infection for several weeks, so it is difficult to determine how to correlate serologic positive evidence of herpes simplex infection.
Three pediatric TINU patients in Korea had favorable renal and uveitis outcomes.[9-11] One patient responded well to topical treatment alone, while two patients achieved remission with a combination of steroid and cytotoxic treatment (azathioprine and cyclosporine, respectively). However, our patient did not achieve complete remission of renal function, and the uveitis did not respond to treatment.
Regusci et al. [4] reported the largest number of pediatric TINU series. In this study, a total of 522 patients received steroids as first-line therapy: topical in 356 cases and systemic in 448 cases. A second-line therapy was reported in 108 patients. Of these, 90 patients were prescribed single or multiple immunosuppressive agents, including methotrexate (n=32), mycophenolate (n=30), cyclosporine (n=19), azathioprine (n=16), cyclophosphamide (n=6), chlorambucil (n=5), and other drugs (n=17). Eighteen patients required hemodialysis. Eleven patients did not receive any therapy. The need for second-line therapy did not appear to be associated with the development of chronic kidney disease (CKD) at follow-up. In fact, of the 108 patients receiving second-line treatment, only 13 (12%) developed CKD. Similarly, among 409 patients not receiving second-line treatments, 82 (20%) (P=0.069 vs. patients not developing CKD).
Saarela et al. [12] postulated that decreased kidney function and/or ocular comorbidities may persist for several years, questioning the previously reported good long-term renal and ocular outcomes of patients with TINU.
Our case was diagnosed when the patient presented with uveitis in moderately advanced nephritis with significant decrease in eGFR and little proteinuria. With treatment, there was an improvement in eGFR and resolution of proteinuria, so we believe there was a response to treating the nephritis, but renal function was not fully restored, contradicting the conventional wisdom that pediatric TINU patients have a good renal prognosis. Overall, our reported outcome was not good because the course of uveitis was not improved and the renal function was not completely recovered, but this was not a case of non-response to treatment.
The clinical course of TINU syndrome in pediatric patients can be variable, and some children with TINU syndrome may have persistent renal dysfunction or uveitis despite initial corticosteroid treatment [13]. This highlights the importance of active therapeutic intervention, including the use of immunosuppressive agents, in pediatric patients with TINU syndrome who do not respond to corticosteroid treatment alone.
The optimal management of TINU syndrome in children is not well established due to the rarity of the disease and limited research in this population. Immunosuppressive agents such as methotrexate, azathioprine, or mycophenolate mofetil have been used in refractory cases of TINU in children, but more research is needed to determine the safety and efficacy of these treatments in this population. TINU syndrome has a genetic basis and an immunological mechanism is involved in pathogenesis. Therefore, long-term monitoring of renal function and uveitis is also essential in the management of pediatric TINU syndrome.
In conclusion, TINU syndrome is a rare disease that can present with uveitis and tubulointerstitial nephritis in children. Clinical outcomes in pediatric TINU syndrome are not always favorable, and active therapeutic intervention, including the use of immunosuppressive agents, may be necessary in refractory cases. Further research is needed to better understand the pathogenesis and optimal management of TINU syndrome in children. Long-term regular monitoring of renal function and ophthalmologic examinations are essential to evaluate treatment response and to detect any recurrence of symptoms or complications.
Notes
Ethical statements
This report was approved by the Institutional Review Board of Konyang University Hospital (IRB No. 2021-01-013) and informed consent was received from the patient parents.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: SIK, EJC
Data curation: SIK, MHP, EJC
Investigation: SIK, EJC
Methodology: SIK, MHP, EJC
Project administration: SIK, EJC
Visualization: SIK, EJC
Writing-original draft: SIK, MHP, EJC
Writing-review & editing: SIK, MHP, EJC
All authors have read and approved the final manuscript.
