Management strategies for congenital isolated hydronephrosis and the natural course of the disease
Article information
Abstract
Congenital isolated hydronephrosis encompasses a spectrum of physiologic states that spontaneously resolve and pathologic obstruction that necessitates surgical intervention. Distinguishing patients whose condition will resolve, those who will require stringent follow-up, and those who will eventually need surgical intervention present a challenge to clinicians, particularly because no unified guidelines for assessment and follow-up have been established. The recognition of the natural course and prognosis of hydronephrosis and a comprehensive understanding of the currently proposed consensus guidelines may aid in multidisciplinary treatment and in providing proper counseling to caregivers. In this review, we aimed to summarize the literature on the grading systems and management strategies for congenital isolated hydronephrosis.
Introduction
Hydronephrosis refers to dilatation of the renal collecting system due to a build-up of urine resulting from drainage problems. Congenital hydronephrosis occurs in up to 1%–5% of all pregnancies [1,2]. More than half of the cases are transient and physiologic, whereas other cases are caused by disorders of the ureteropelvic junction (UPJ) including intrinsic stenosis (10%–30%), vesicoureteral reflux (VUR; 10%–30%), and congenital anomalies leading to secondary dilatation of the urinary tract [1,3,4]. To date, studies have shown that low-grade isolated hydronephrosis usually resolves during the first few years of life [5,6], whereas high-grade hydronephrosis requires intervention to prevent the progression of obstruction or deterioration of renal function [7].
Distinguishing children who require follow-up or intervention, determining the possibility of resolution and the time to resolution, deciding about performing pyeloplasty to relieve the obstruction and determining the timing of the procedure, and preserving the patient’s renal function are crucial issues for both clinicians and family members. To stratify the risk of early surgical intervention or the possibility of resolution, attempts have been made to create a unified grading system for urinary tract dilatation that can be used during the prenatal or postnatal period; however, no definitive consensus guidelines have been established to date [8].
In this review, we aimed to summarize the literature (to date) on the proposed grading systems and management strategies for congenital isolated hydronephrosis, as well as to describe the natural history.
Detection and classification–grading systems
Currently, no standardized protocol exists for defining, classifying, and grading congenital hydronephrosis. Different terminologies with overlapping meanings are used to describe the status of dilatation (e.g., pelviectasia, pelviectasis, hydronephrosis, and urinary tract dilatation), and different clinicians from different subspecialties (e.g., pediatric urology, pediatric radiology, pediatric nephrology, and obstetrics) may use the terms to refer to different conditions [9,10]. Consequently, several grading systems have been developed, leading to the use of various nomenclatures and causing a misunderstanding between the radiologist and the clinician [11]. In this context, we will review the most widely used and the recently proposed grading systems aimed at providing a unified classification during the perinatal period, including their validation in the literature.
Society for Fetal Urology classification
In 1993, the Society for Fetal Urology (SFU) proposed a 5-point numeric grading system (0–IV) based on the postnatal appearance of the renal pelvis, calyces, and renal parenchyma on ultrasonography (USG) images (Fig. 1) [1,6,12]. The SFU classification remains the most widely used grading system owing to its intuitiveness and ease of use, especially in cases of isolated hydronephrosis. However, interobserver and intraobserver variabilities exist owing to the nature of morphologic classification. Furthermore, since it was not originally developed for use in antenatal evaluation, it has not been widely adopted in subspecialties other than pediatric urology radiology (e.g., obstetrics and neonatology).
Grading based on the anteroposterior pelvic diameter
Anteroposterior pelvic diameter (APD) measurement, obtained from a transverse section of the renal hilum, is also widely used by itself or in conjunction with SFU grading. APD is an objective quantitative parameter widely used as a predictor of pathology and outcome, as well as of the resolution of the condition or the need for an intervention [1,8,13]. However, it also has limitations. Because APD measurement does not provide descriptive details of the renal parenchyma, calyces, ureter, and lower urinary tract, it does not accurately reflect the degree of hydronephrosis according to different renal pelvic configurations. Some studies argue that there is no threshold separating nonobstructive from obstructive dilatation of the kidney because renal dilatation is affected by many factors (e.g., hydration status, bladder filling, position, and respiration of the patient) giving its dynamic character [11,14]. Because of the advantages and disadvantages of both grading systems, SFU grading and APD measurement are commonly used together complementarily in clinical practice. As the authors have previously demonstrated, in cases showing a discrepancy between morphologic classification and APD measurement (i.e., higher grade in the SFU classification than that based on APD measurement), the resolution time should be predicted using the APD measurement rather than the SFU grade [15]. This is because normalization of morphology occurs before improvement in the APD measurements.
Urinary tract dilation classification system
The urinary tract dilation (UTD) classification system was developed in 2014 as a collaborative effort among eight different medical and surgical societies (American College of Radiology, American Institute of Ultrasound in Medicine, American Society of Pediatric Nephrology, SFU, Society for Maternal-Fetal Medicine, Society for Pediatric Urology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound) in an attempt to establish a standardized and simplified description of hydronephrosis that can be consistently applied across specialties for prenatal and postnatal evaluation and management [8,16]. This classification includes parameters such as the APD of the renal pelvis (normal, <10 mm), presence of central and peripheral calyceal dilatation, renal parenchymal abnormalities, ureteral abnormalities, and bladder abnormalities in two antenatal (UTD-A1 and UTD-A2) and three postnatal (UTD-P1, UTD-P2, and UTD-P3) categories (Fig. 2). This system is intended to stratify the risk of postnatal uropathies and the clinical outcomes and to conduct a cost-effective evaluation in high-risk patients rather than being a mere descriptive grading system [8,17]. However, the system may also cause confusion because the classification suggests the general term “urinary tract dilatation” to indicate all types of ureteral and kidney dilatation, including UPJ obstruction (UPJO), ureterovesical junction-type hydroureteronephrosis, VUR, bladder pathologies, and posterior urethral valve formation. Its additional limitations include interrater discrepancy in the assessment of calyceal dilatation, the wide range encompassed by the UTD-P3 grade, and the complexity and time-consuming nature of its application in real clinical practice [11]. Nonetheless, some studies have validated the usefulness of the UTD grading system in predicting the need for surgical intervention or predicting urinary tract infection by showing a relationship between UTD grade and clinical outcomes [17-24].
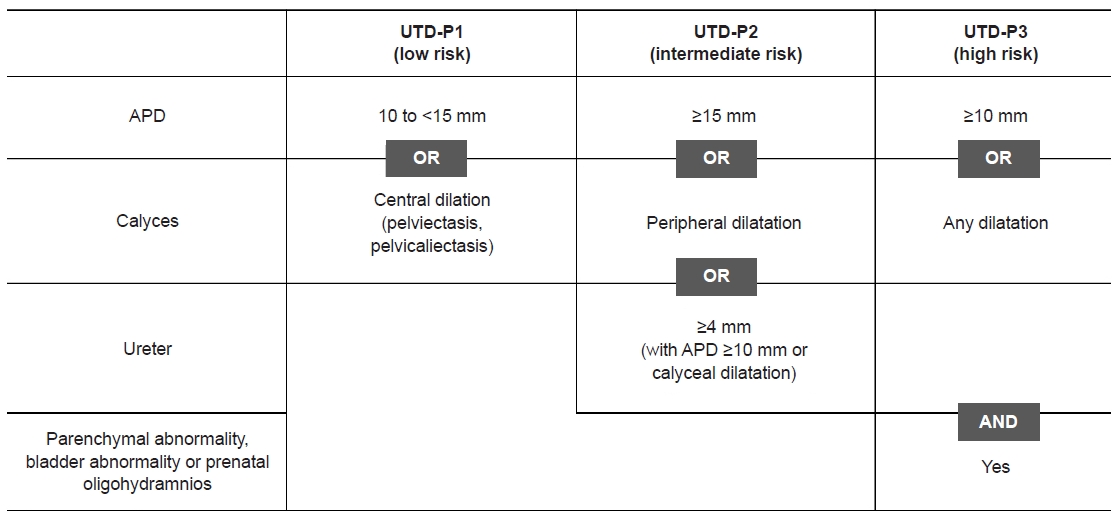
Urinary tract dilation (UTD) classification system (postnatal categories). Although the UTD classification system has two antenatal categories (UTD-A1 and UTD-A2–3) and three postnatal categories (UTD-P1, UTD-P2, and UTD-P3) [8,16], only the postnatal categories (>48 hours) are presented here. APD, anteroposterior pelvic diameter. Adapted from Nguyen et al. [16] with permission from Springer.
Onen grading system
The Onen system was developed in 2007 for the assessment of prenatal and postnatal hydronephrosis with UPJ pathology, with emphasis on the quality of the renal parenchyma, and was updated in 2016 [11,25]. It is based on nonsubjective parameters (presence of dilatation of the pelvicalyceal system and quality of the renal parenchyma based on exact criteria) (Fig. 3). Although the system is not widely used because of low recognition by practitioners, a few groups have recently reported its low subjectivity with a decreased interobserver agreement in Onen grades 2 to 3 [26,27].
Among the aforementioned grading systems, the SFU classification of congenital hydronephrosis seems to remain the most widely used classification system by clinicians owing to familiarity and established practice patterns, followed by APD measurement and the UTD system [17,28,29].
Risk-based management and follow-up plan after birth
As previously mentioned, no universal guideline exists on the frequency and timing of USG examination and the required duration of follow-up. In addition, heterogeneity in clinical management exists among pediatric radiologists, pediatric urologists, and maternal-fetal obstetricians, partly because of the lack of prospective studies and different practices across different centers [10]. This section will cover the postnatal management of congenital hydronephrosis according to the current literature in the context of clinical decision-making (Fig. 4).

Suggested follow-up and management strategies for congenital isolated hydronephrosis. The diagram summarizes the proposed guidelines from the literature. USG, ultrasonography; SFU, Society for Fetal Urology; UTD, urinary tract dilatation; DRS, diuretic renal scan; VCUG, voiding cystourethrography; prn, pro re nata.
For unilateral hydronephrosis, postnatal evaluation should begin within the first week (after the second day, usually from the fifth to seventh days, to ensure adequate hydration) of life using renal USG. For bilateral hydronephrosis, early postnatal imaging is recommended. After the initial evaluation, follow-up and management are stratified according to severity, as assessed using the aforementioned grading systems.
In cases of known prenatal hydronephrosis that show normalization on the first postnatal USG, the follow-up may be terminated. However, 15% to 45% of patients with normalized initial USG results show abnormal USG results on follow-up, suggesting the need for a second USG examination at 1 to 6 months of age (varying among studies) despite normal findings on the first USG [1,14,30,31].
In the case of mild hydronephrosis (generally grade I and unilateral grade II in SFU grading and UTD-P1), observational studies anecdotally recommend less aggressive imaging follow-up [14,31], or no further follow-up [32], owing to the nature of spontaneous resolution during the first 2 to 3 years [15,19,33]. Irrespective of the suggestions, an APD of approximately 10 to 20 mm (cutoff value may vary among studies) can be managed conservatively [14,15,34]. Follow-up evaluations using USG after 3 to 6 months for the first year, every 6 months until 3 years, and every 1 to 2 years thereafter (or according to the symptoms [flank pain, dysuria] articulated by the patient) are usually recommended [8,14,31]. Although extremely rare, late worsening after spontaneous resolution can occur in some patients (1%–5%) in a few months (up to 5–6 years) [35], even in patients with mild congenital hydronephrosis [1,33,36]. Clinicians should be aware of this possibility and educate the patients and caregivers about the possible need for follow-up imaging in intervals (varying from 1 to 6–12 months among studies) after resolution or when symptoms such as abdominal pain and urinary symptoms appear [1,8,14,36-38].
For moderate hydronephrosis with an intermediate risk of progression (bilateral SFU grade II, SFU grade III, and UTD-P2), a second USG examination is recommended in the first month and every 1 to 3 months thereafter, during the first year, depending on the stability of the patient’s condition. For the next 2 years, follow-up every 6 months is recommended. Annual follow-up or follow-up according to the symptoms (flank pain and dysuria) articulated by the toddler until 6 years is also recommended [8,14,31]. Diuretic renal scan (DRS), which can be performed from 6 to 8 weeks of age, is the most commonly used modality for assessing the presence of upper urinary tract obstruction in infants. It is usually recommended when two renal USG examinations, during at least 3 months, show no improvement or suggest the aggravation of moderate hydronephrosis. The indications for voiding cystourethrography (VCUG) include bilateral hydronephrosis, ureteral dilatation, abnormal renal echogenicity, and abnormal appearance of the bladder, which are suggestive of lower urinary tract disease (e.g., posterior urethral valve or VUR) [5]. However, the decision to recommend DRS or VCUG is dependent on the clinician’s discretion because less invasiveness and cost-effectiveness in evaluation are recently being emphasized, supported by the fact that most patients remain asymptomatic without severe pathology [8,31]. Duong et al. [39] suggested that DRS should only be performed in patients with APD ≥30 mm, major calyceal dilatation (>10 mm), or renal parenchymal thinning and emphasized the need for more conservative management among patients with mild-to-moderate hydronephrosis.
For severe, high-risk hydronephrosis (SFU grade IV, UTD-P3), USG examination should be repeated at 1 month, followed by DRS at age 6 to 8 weeks [8,31]. The possibility of a later follow-up using USG examination and DRS/VCUG depends on the results of second USG with DRS, and the plans for surgery. The index of obstructive uropathy (UPJO) and the indications for surgical intervention will be addressed later.
Natural course of isolated hydronephrosis
According to existing studies, >50% to 70% of all cases of isolated hydronephrosis resolve regardless of the grade [5,6,15,40]. The resolution rate differs according to the baseline severity of hydronephrosis. Prior studies on low-grade hydronephrosis (SFU grades I–II and APD <10–20 mm) showed resolution or improvement in 56.0% to 97.4% of the cases, implying a benign condition [6,41,42]. Elmaci and Donmez [13] evaluated the congenital hydronephrosis’s time to resolution in patients with APD <20 mm; those with APD <10 mm showed complete resolution in a median of 5 months, whereas those with an APD of 10 to 20 mm showed complete resolution in a median of 11 months. In addition, cumulative resolution rates were reported by several prospective and retrospective studies. In a prospective study, Braga et al. [19] reported the cumulative resolution rate at 3 years for each grade in the SFU and UTD systems (98% for SFU I, 87% for SFU II, 76% for SFU III, and 56% for SFU IV; 90% for UTD-P1, 81% for UTD-P2, and 71% for UTD-P3). In addition, the authors previously reported the cumulative resolution rates of isolated hydronephrosis at 2 years in a retrospective study (81.7%, 65.6%, 37.6%, and 5.2% for SFU grades I, II, III, and IV, respectively) [15]. Among cases of high-grade hydronephrosis associated with UPJ stenosis, approximately 27% show resolution, >50% remain stable, and the rest progress with possible renal function deterioration [3]. Surgical intervention has been required in approximately 25% of all cases, ranging from 5% to 50% depending on the study [1,15,43-46]. Therefore, after at least 2 to 3 years of watchful observation and evaluation, termination of follow-up may be possible since the outcome would be determined within these years.
Prediction and decision of intervention
Disagreements about the definition of obstruction and the indications and timing of surgery in hydronephrosis due to UPJO remain. The appearance of symptoms of UPJO, such as pain and urinary tract infection, is indicative of the need for surgery. A differential renal function of <40% with impaired drainage (T½ >20 minutes) on DRS or a >10% deterioration of renal function on a serial renal scan is also generally considered a surgical indication [6,31,38,47].
Additional studies have presented the predictors of surgery and their corresponding cutoff values, including initial postnatal APD, cortical tissue transit time on DRS, renal pyramidal thickness, and renal parenchyma-to-hydronephrosis area ratio (PHAR) [34,47-51].
Initial postnatal APD
Postnatal APD has been widely used as an index for evaluating and anticipating the presence of obstruction, with advantages of wide availability and absence of radiation exposure. In clinical practice, sequential changes in APD are mainly used to determine management plans. Although no absolute cutoff value of APD for performing pyeloplasty has been defined, several studies suggested different APD values, ranging from 15 to 30 mm, as significant predictors of surgical intervention [8,34,37,50,52]. Arora et al. [47] performed a prospective multivariate analysis and showed that an APD of up to 24 mm in the first week after birth can predict the need for surgical intervention (sensitivity, 73.1%; specificity, 88.0%). The prospective cohort studies of Coelho et al. [37] and Dias et al. [34] suggested an APD of >15 and 18 mm as the cutoff value, respectively.
Delayed tissue transit time in 99mTc-mercaptoacetyltriglycine DRS
Some recent studies have shown that delayed tissue transit time, which is defined as an absence of activity in the subcortical structures or in the pelvis on a 99mTc-mercaptoacetyltriglycine (MAG3) DRS within 3 or 8 minutes of tracer injection, can predict deterioration of UPJO in pediatric populations [51,53-55]. Song et al. [56] proposed that delayed tissue transit time on 99mTc-MAG3 DRS is a significant predictor of renal function improvement after pyeloplasty in patients with UPJO. Therefore, they suggested that delayed tissue transit time should be considered a candidate predictor of immediate pyeloplasty and decreased differential renal function.
Renal pyramidal thickness
The renal pyramid is the first portion of renal parenchyma that becomes affected in high-grade hydronephrosis. The parenchymal thickness changes with age, making its clinical application difficult in a growing child. In contrast, the renal pyramid is a part of the parenchyma that grows slowly and shows only small changes in the first 9 years of life; thus, it is a feasible parameter for evaluation and comparison between serial USG images [57]. Pyramidal thickness measurement was not previously performed in patients with hydronephrosis until Hodhod et al. [48] recently measured pyramidal thickness in the supine position in the middle third of the sagittal plane. In their study, multivariate analysis showed that a renal pyramidal thickness of ≤3 mm (sensitivity, 98.1%; specificity, 89.7%) predicted the need for surgical intervention.
Renal PHAR
Some studies have attempted to simultaneously measure the renal parenchymal volume and the grade of hydronephrosis using USG (without a renal scan) as a surrogate of renal function in patients with hydronephrosis [49,58]. In this regard, Rickard et al. [49] showed that the renal PHAR predicted the need for surgery (cutoff value, <0.5) in high-grade hydronephrosis (area under the receiver operating characteristic curve, 0.816; P<0.001) more efficiently than the APD measurement, SFU grade, and UTD classification.
Risk of urinary tract infection
The existing studies commonly suggest that the risk of urinary tract infection increases with the degree of hydronephrosis. Observational studies have shown that patients with moderate or severe hydronephrosis show an increased incidence (13.8%–40.0% for moderate-to-severe hydronephrosis vs. 4.1%–14.0% for mild hydronephrosis) of urinary tract infection [37,59-61]. Patients with hydronephrosis with obstructive drainage patterns on renal scans, without VUR, have a higher risk than those without obstructive patterns [61-63]. Furthermore, in terms of the benefits of antibiotic prophylaxis, different outcomes have been reported. Braga et al. [64,65] demonstrated a protective effect of antibiotic prophylaxis, especially in patients with high-grade hydronephrosis, in their systematic review and meta-analysis, whereas Estrada et al. [66] showed significant improvement in infection after prophylaxis even in patients with mild hydronephrosis. In clinical practice, the use of prophylactic antibiotics remains nonuniform owing to the absence of recommendations or guidelines from randomized control studies [67,68]. An ongoing randomized control trial on hydronephrosis with UPJO-like and non-refluxing megaureter by Braga et al. (Clinical Trials Registry no. NCT01140516) might aid in elucidating the effect of chemoprophylaxis. Therefore, clinicians are currently advised to decide whether they want to make use of antibiotics on a case-by-case basis while keeping in mind that high-grade hydronephrosis may confer an increased risk of urinary tract infection.
Conclusions
Predicting the natural course of prenatally detected hydronephrosis has become possible with increasing knowledge and accumulated outcomes from cases treated with surgical intervention. Since no definite consensus exists about using a certain grading system in clinical practice, a practical, user-friendly system, combined with the use of an objective imaging modality that is generally accepted by multidisciplinary specialists, is needed. Furthermore, the establishment of the timing of the initial evaluation and follow-up intervals according to disease severity can aid in efficient management and help inform the caregivers and patients about the prognosis and follow-up plans.
Notes
Conflicts of interest
Joo Hoon Lee is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Author contributions
Conceptualization: YSP, KSK
Data curation: JJ, JHL
Investigation: SHS
Methodology: HMY, YAC, DHM
Project administration: YSP
Visualization: SHS, HMY, YAC, DHM
Writing-original draft: JJ
Writing-review & editing: JWJ, JHL, YSP, KSK
All authors read and approved the final manuscript.


