Introduction
Obstructive uropathy is one of the causes of acute kidney injury in children if the obstruction occurs in a single kidney, if it involves both ureters, or if urethral obstruction is observed [1]. The most common obstructive uropathy in children is congenital malformation, such as posterior urethral valves and bilateral ureteropelvic junction obstruction [2]. Malignant pelvic masses obstructing the ureter are widely reported in adults but are rarely observed in children [3]. The treatment of a ureteral obstruction related to pelvic malignancy is a therapeutic challenge, with a median survival period of 3ŌĆō7 months in adults [4]. However, better outcomes were noted for pediatric patients with pelvic malignancy leading to ureteral obstruction than for adult patients, with a 5-year mortality rate of 20% being reported for pediatric patients [5]. Therefore, urgent ureteral decompression, such as nephrostomy, ureterostomy, or double J stent implantation should be initiated immediately for the treatment of acute kidney injury in children with a malignant pelvic tumor obstructing the urinary tract and should be prioritized as highly as emergency hemodialysis. Here, we report a rare case of bilateral ureteral obstruction associated with pelvic rhabdomyosarcoma presenting with acute kidney injury successfully treated by ureteral diversion with restoration of good renal function.
Case report
A previously healthy 15-year-old female presented with a 2-week history of weak urinary stream and hesitancy. She was admitted to a different hospital with complaints of general weakness and vomiting on January 18, 2012.
She looked ill. The initial vital signs recorded at the other hospital were as follows: blood pressure (BP), 130/80 mmHg; pulse rate, 74 beats/min; respiratory rate, 20 breaths/min; and body temperature, 36.7Ōäā. Her body weight was 86 kg; this was 5ŌĆō6 kg more than her usual weight. The pupil reflex was prompt, and anemia was not detected in both conjunctivae. The cervical lymph node was not palpable. A skin rash was not observed. She had no specific abdominal tenderness, and the costovertebral area was more tender on the right than on the left. She had no pitting edema. The left inguinal lymph nodes were palpable.
The laboratory findings on admission to this hospital were as follows: white blood cell (WBC) count, 13,500/╬╝L (segmental neutrophil 81.3%, lymphocyte 13.6%); hemoglobin level, 12.1 g/dL; hematocrit volume, 34.5%; platelet count, 411,000/╬╝L; albumin level, 4.1 g/dL; total protein level, 7.1 g/dL; aspartate aminotransferase level, 18 IU/L; alanine aminotransferase level, 11 IU/L; blood urea nitrogen (BUN) level, 96 mg/dL; creatinine (Cr) level, 17.13 mg/dL; sodium level, 142 mmol/L; potassium level, 4.8 mmol/L; chloride level, 101 mmol/L; bicarbonate level, 8.7 mmol/L; calcium level, 8.8 mg/dL; phosphorus level, 7.0 mg/dL; and uric acid level, 13.4 mg/dL. C-reactive protein levels were 4.45 mg/dL. The results for urinalysis with microscopy were as follows: specific gravity, 1.015; pH, 5.0; protein, 1+; blood, 4+; glucose, negative; ketone, trace; red blood cell count, 6ŌĆō9/high-power field (HPF); and WBC count, 10ŌĆō29/HPF. The urine protein to Cr ratio was 0.25 g/g Cr.
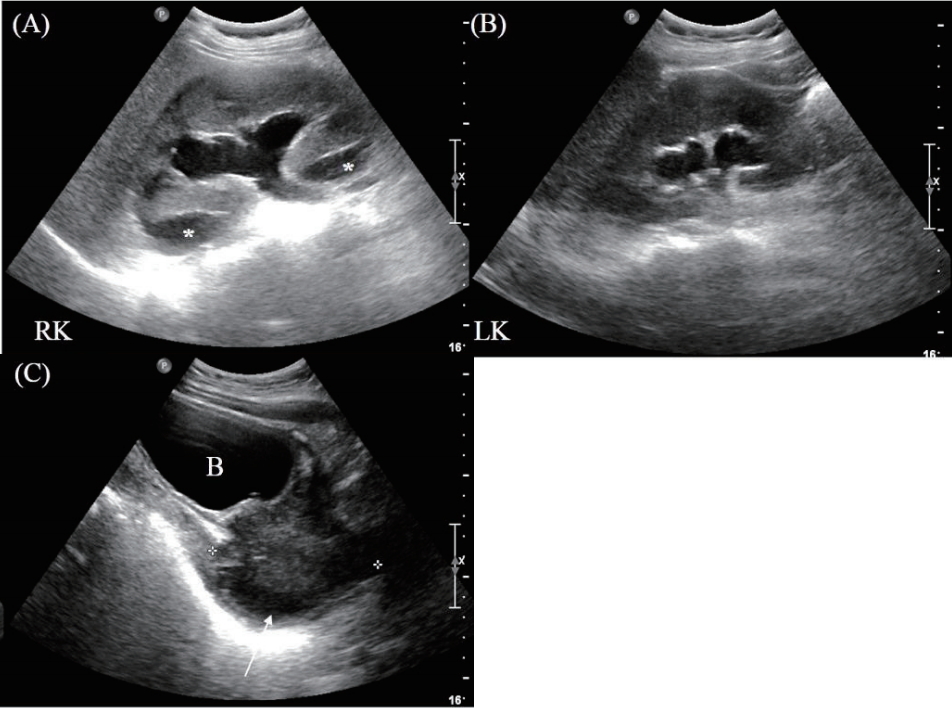
Initially, we suspected acute kidney injury, and she was treated with acute hemodialysis. Additional blood tests and kidney sonography were performed to determine the cause of azotemia; the results of these analysis were as follows: immunoglobulin (Ig) G level, 1153 mg/dL (normal, 680ŌĆō1,620 mg/dL); IgA level, 144 mg/dL (normal, 84ŌĆō438 mg/dL); IgM level, 119 mg/dL (normal, 57ŌĆō288 mg/dL); complement C3 level, 153 mg/dL (normal, 65ŌĆō135 mg/dL); C4 level, 39.7 mg/dL (normal, 13ŌĆō35 mg/dL); hepatitis B virus surface antigen (HBsAg), negative; antibodies against hepatitis C virus (anti-HCV), negative; antibodies against human immunodeficiency virus (anti-HIV), negative; cryoglobulin, negative; antistreptolysin O level, 170 IU/ml (normal, <200 IU/ml); antineutrophil cytoplasmic antibody (Ab), negative; and antinuclear Ab, negative. Kidney sonography revealed diffuse bilateral hydronephrosis with globular renal swelling and small subcapsular fluid indicative of urinoma in the right kidney; a lobulating contour mass-like lesion in the posterior aspect of the bladder involving the urethra and vagina was also observed (Fig. 1).
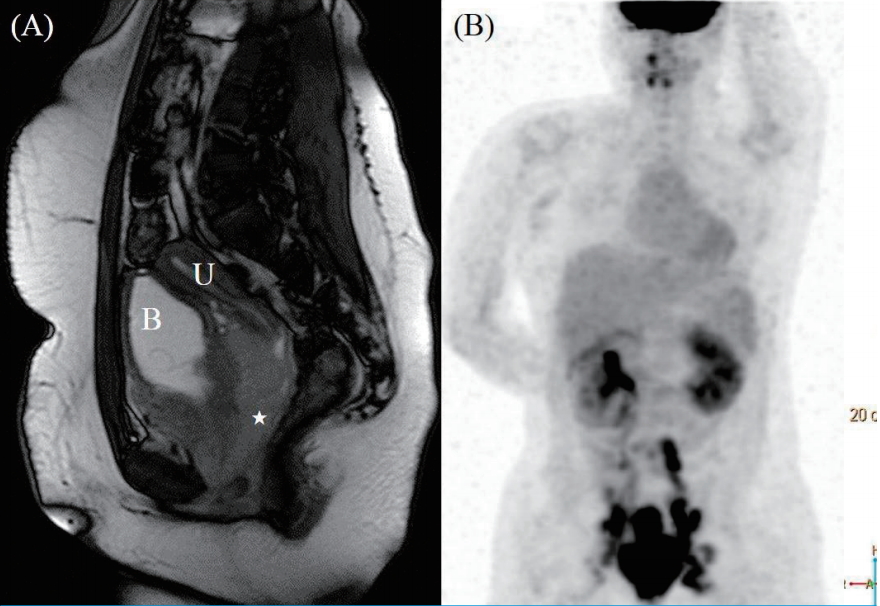
She was transferred to a tertiary hospital for the evaluation of the pelvic mass and management of acute kidney injury. When she was transferred, double J catheter insertion was attempted on both sides of each obstructed urinary system to resolve the acute kidney injury, but the insertion on the right side was not successful. However, the renal function rapidly improved with BUN levels of 12.7 mg/dL and Cr levels of 1.2 mg/dL, and emergency hemodialysis was performed 5 times and then discontinued. Magnetic resonance imaging (MRI) and positron emission tomography (PET) were performed (Fig. 2). An excisional biopsy was performed on the left inguinal lymph node.
Immunohistochemical staining results were as follows: the samples stained positive for desmin, but were negative for cytokeratin, leukocyte common antigen, and smooth muscle actin. The CD99 and FLi-1 tests performed to differentiate the Ewing sarcoma family were also negative. As the sample showed negative chromogranin and synaptophysin findings, the possibility of neuroendocrine tumors was also excluded. Hence, the tissue findings were consistent with those of a rhabdomyosarcoma.
She was transferred to our hospital to receive chemotherapy closer to home. Starting February 11, 2012, she was treated with the Intergroup Rhabdomyosarcoma study-IV (IRS IV) protocol. The IRS IV protocol is a treatment wherein radiation therapy is combined with chemotherapy, including vincristine, dactinomycin, cyclophosphamide, and mesna [6].
According to the protocol, she received 3 cycles of vincristine, dactinomycin, and cyclophosphamide (VAC) between February 11, 2012 and April 26, and showed partial response (PR). On March 23, 2012, the double J catheter in the left ureter was removed. Vincristine and cyclophosphamide (VC) administration followed by pelvic radiation therapy were performed according to the protocol during the period from May 5, 2012 to June 27, 2012. She underwent bilateral ovarian transposition surgery for fertility preservation under gynecologic consultation before receiving pelvic radiotherapy. At the time of surgery, the uterus was found to be in the normal state. Both ovaries were fixed by suturing on the upper abdominal wall, which was not affected at a fixed radiation dose of 50.4 Gy/28 Fx between May 20, 2012 and July 20, 2012.
After radiotherapy, VAC chemotherapy was performed again during the period from August 8, 2012 to March 19, 2013, and all treatments were completed. At this time, an imaging test was performed to evaluate the response, and the result was complete response (CR). The patient is followed-up regularly with chest low dose computed tomography and pelvic MRI. As of 2019, the patient has been relapse-free for 7 years and normal renal function with the level of serum creatinine, 0.79 mgdL.
Discussion
There were some differences in the reports on cancers that cause malignant ureteral obstruction. In adults, advanced carcinoma of the stomach, colon, and the gynecologic and urologic systems were the common neoplasms [7,8]. Based on these studies, gastrointestinal cancer was considered to be the most common cause of malignant ureteral obstruction in adults.
In contrast, a slightly different pattern was observed in children. In children with malignant ureteral obstruction, rhabdomyosarcoma, Ewing's sarcoma, neuroblastoma, lymphoma, teratoma, and desmoplastic tumors were the most common neoplasms [3,5,9]. Although rare, mucinous cystoadenoma of the ovary was likely to cause extrinsic ureteral obstruction in children, and approximately 20 cases have been reported [10].
Therefore, very poor prognosis was noted for malignant ureteral obstruction in adults. The average life expectancy was less than 1 year [7]. Furthermore, a renal function recovery rate of 42ŌĆō44% was reported after the resolution of malignant ureteral obstruction [11,12]. However, the overall survival rate of children with malignant ureteral obstruction was approximately 70%, indicating that the prognosis of children was better than that of adults [3, 13]. A much better renal function recovery rate was reported as well, with normalized serum Cr levels in most of children with malignant ureteral obstruction who had renal failure on presentation [3]. The reversibility of renal function is associated with better preservation in children than in adults, which is related to several factors, such as incomplete and short-duration obstruction [3]. Diffuse and severe tubular atrophy with interstitial fibrosis in renal biopsy were indicated in adults with malignant ureteral obstruction [12]. These histologic findings may be aggravated in proportion to the obstruction period, thus, affecting the renal prognosis.
In our patient, urinary diversion was performed by bilateral insertion of a double J (DJ) catheter; however unilateral DJ catheter insertion was unsuccessful. However, urinary diversion had a positive effect on survival and renal function, in addition to surgical resection, chemotherapy, and radiation therapy for rhabdomyosarcoma in this patient. According to another study, nephrostomy (n=12), DJ stent implantation (n=3) and ureteroureterostomy with tumor resection (n=2) were performed in 17 children with pelvic tumors [3]. Urinary tract infection was the most common complication of urinary diversion, and mechanical problems, such as tube dislodgement and obstruction were reported [3].
In conclusion, in children with malignant urinary obstruction, urgent ureteral decompression, such as nephrostomy, ureterostomy, or DJ catheter insertion should be initiated immediately for the treatment of acute kidney injury and should be prioritized as highly as emergency hemodialysis. Ureteral diversion can restore renal function in addition to surgical resection, chemotherapy, or radiation therapy for bilateral ureteral obstruction associated with pelvic tumors.
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print