Effects on Quality of Life in Patients with Neurogenic Bladder treated with Clean Intermittent Catheterization: Change from Multiple Use Catheter to Single Use Catheter
Article information
Abstract
Purpose
To evaluate changes in quality of life (QoL) in patients with neurogenic bladder treated with clean intermittent catheterization (CIC), who changed from a multiple use catheter (MUC) to single use catheter (SUC).
Methods
The Modified Intermittent Self-Catheterization Questionnaire (mISC-Q) was used to determine potential changes in patients’ QoL as a result of switching from MUC to SUC. The mISC-Q consists of questions within four categories: ease of use, convenience, discreetness, and symptomatic benefit. Answers were graded as Strongly agree (+2), Agree (+1), Not sure (0), Disagree (-1), and Strongly disagree (-2). Overall patient QoL, as well as by sex, disease (presence of augmentation cystoplasty), and catheterization route (via urethra or urinary diversion), were analyzed.
Results
Thirty-eight patients (21M:17F; mean age: 21.7±5.3 y) submitted questionnaires. For ease of use, SUC was significantly better than MUC (score: 0.364, P=0.002) in all patients. Patients with catheterization via the urethra showed significant favor for SUC in ease of use (score: 0.512, P<0.001) and convenience (score: 0.714, P=0.011), but patients with catheterization via the abdominal stoma of urinary diversion gave negative scores in all categories, though no categories were significant.
Conclusion
This study suggested that changing from MUC to SUC may lead to improvements in QoL, especially regarding ease of use. This benefit was clearly found in patients with catheterization via urethra rather than abdominal stoma of urinary diversion.
Introduction
Clean intermittent catheterization (CIC) of neurogenic bladder patients has become the gold standard treatment since Lapides et al. first introduced CIC as a safety procedure in 1971 [1]. However, many patients stop CIC because it is hard to maintain, as well as other reasons including lack of understanding, infection, complication, and pain [2]. The most important factor for CIC is proper education that includes accurate procedure, management of the catheter, how to handle complications from CIC, and the system of follow-up. Nowadays, most neurogenic bladder patients complete CIC with a reusable catheter [3], even though a disposable catheter is available.
According to previous studies by Kanaheswari et al. [3] and Schlager et al. [4], there is still controversy regarding urinary tract infection incidence between disposable and multiple use catheterization. However, Morris and Schulz reported that patient compliance is an essential contributing factor in the management of chronic illness, such as neurogenic bladder management [5]. From the perspective of the patient, factors such as ease of use or convenience may play a more important role than incidence of symptomatic urinary tract infection.
In patients with CIC that are suspected of having bacteriuria, CIC should be continue, except when bacteriuria is accompanied with fever and acute pyelonephritis. Most urologists are aware that urinalysis and urine culture are nonessential examinations for asymptomatic bacteriuria in patients with continuous CIC [6]. However, the presence or absence of CIC is the most important factor for neurogenic bladder patients. Most patients with CIC in the neurogenic bladder have high-pressure bladder concurrently with detrusor sphincter dyssynergia, involuntary detrusor contraction, and/or poor compliance that cause upper tract damage if bladder emptying is not achieved [7]. The continuation of CIC is thus a very important issue, and choosing convenient catheterization is an important way to reduce complications.
The multiple use catheter (MUC) has a hydrophilic polymer coating that absorbs and binds to water, resulting in a slippery surface that ensures complete lubrication as the catheter is passed through the urethra into the bladder. It has been suggested that the use of hydrophilic-coated catheters may lower the risk of long-term urethral complications that otherwise may have been exacerbated by repeated insertions of a catheter [8]. Conversely, the tube of a sterile single use catheter (SUC) is made from polyurethane that is free from PVC and phthalates, which are components of traditional MUCs. Polyurethane catheters have a better level of stiffness compared to those made from PVC or phthalate.
Even though medical insurance covers the use of SUC for each void, the majority of patients reuse the MUC due to economic reasons [4]. MUCs are prone to infection and are difficult to manage. Due to these problems, performing CIC using MUC may negatively affect the patient’s quality of life (QoL). Therefore, this study examined the changes in QoL in patients with neurogenic bladder treated with self-catheterization, who changed from MUC to SUC.
Material and methods
Forty-five pediatric patients, who underwent CIC for neurogenic bladder of various etiologies, were selected from the Pediatric Urology Department at Seoul National University Hospital between January 2016 and June 2016. Each patient previously performed CIC using MUC and recently changed to SUC, and the response of this change was evaluated by asking each patient to fill out a questionnaire [9].
Changes in QoL were assessed using the Modified Intermittent Self-Catheterization Questionnaire (mISC-Q) [10,11]. Questions regarding ease of use, convenience, discreetness, and symptomatic benefit were graded using the following answers: Strongly disagree, Disagree, Not sure, Agree, and Strongly agree. The mISC-Q was translated into Korean by the author; no separate adjustment process was performed before its use.
Each answer was weighted using a numeric value from -2 to +2 (with -2 coinciding with Strongly disagree and +2 coinciding with Strongly agree), and established a standard by zero which made no difference between two methods. Means of each category calculated as the total score. Chi-square test and Fisher's exact test were used for categorical variables. Each survey category was first analyzed using descriptive statistics and then analyzed for differences between the two groups. Paired t-test was used to calculate the mean, standard deviation and P-value of each survey category. All statistical analyses were performed using SPSS (IBM). All statistical tests were 2-sided, and P-values of ≤ 0.050 were considered to be significant.
Results
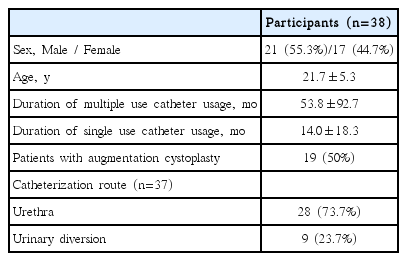
Of the 45 patients enrolled in this study, only 38 patients completed the questionnaire. Patient characteristics are presented in Table 1. Changes in patient QoL as a result of changing from MUC to SUC are presented in Table 2. Values are presented as an index score reflecting favor towards single catheter than multiple use catheter. In all participants, SUC was significantly better than MUC for ease of use. Additionally, both male and female patients reported a significant improvement in ease of use only. Although patients with history of previous augmentation cystoplasty did not report a significant change in ease of catheterization, patients without augmentation history reported significant improvements in ease and convenience after changing to SUCs [12]. Patients performing CIC via urethral catheterization showed improved ease of use and convenience. Additionally, although patients performing catheterization via abdominal urinary stoma of urinary diversion reported lower questionnaire scores overall, the results were not statistically significant.
Discussion
Since the introduction of CIC as a safe alternative for bladder emptying, CIC has become the first-line and preferred method of drainage in patients with neurogenic bladder dysfunction [13]. This study evaluated changes in QoL parameters in patients with neurogenic bladder that switched from using MUC to SUC as SUC is becoming more common practice.
With regard to the questionnaire categories, most patients in this study gave high scores for ease of use. This suggests that SUC is easier to carry than MUC and does not require jelly for lubrication and disinfection devices. Also, since SUC is discarded after use, patients do not need a separate container to keep the used catheter.
Additionally, the majority of patients, except for urinary diversion patients, gave high scores for convenience, likely because the questions ask about ownership of the home. Unlike MUC, SUC can be stored in several places and small quantities, and patients may not forget where the catheter was stored.
Further, due to the characteristics of SUC, it was expected that catheter portability and cost would be disadvantageous. However, the results were better than expected, except for urinary diversion patients, because most of the surveyed patients’ medical expenses were covered by health insurance and other sources, and SUCs are individually packed and the patient can only carry as many as actually needed.
Patients with catheterization via urinary diversion did not present significant results, and in most cases, the MUC received higher scores. This is probably due to the inconvenience of SUC for these patients, who are already accustomed to the existing catheterization method and the nature of the abdominal stoma.
As a result, patients in all groups, except urinary diversion patients, gave higher scores in favor of SUC in all four categories (ease of use, convenience, discreetness, and symptomatic benefit), even though they may or may not have been significant. However, in female patients, the score was lower in the symptomatic benefit category, likely due to symptoms of cystitis, which can easily occur in female patients because of their urethral anatomy.
Limitations of our study mainly arose from the fact that patient satisfaction scores depended only on a 5-point scale. For example, for improved ease of use, convenience, discreetness, and symptomatic benefit, 2 points were given if the patient strongly agreed, and 1 point if the patient agreed, which may not have accurately reflected a two-fold quantitative improvement for the actual subjective improvement; the same can be inferred for negative reactions. Regardless, our study provides valuable insight into subjective factors, such as ease of use and convenience, that may guide patients in making decisions about their self-catheterization options. Additionally, this study not only investigated patients with urinary tract infections by different sex, disease, and CIC route, but also examined changes in patients’ QoL as a result of changing from reusable to disposable catheters.
In conclusion, this study suggested that changing the CIC method from MUC to SUC may lead to improved patient QoL, especially in ease of use. This benefit was clearly shown in patients with catheterization via the urethra rather than the abdominal stoma of urinary diversion.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.