| Child Kidney Dis > Volume 22(2); 2018 > Article |
|
Abstract
Nutcracker syndrome is a phenomenon that the left renal vein (LRV) is pressed between the superior mesenteric artery (SMA) and the aorta. Clinical characteristics include gross or microscopic hematuria, orthostatic proteinuria, abdominal pain, and back pain. It occurs due to LRV squeezing caused by narrowed aortomesenteric angle. SMA syndrome is a disease that the third part of the duodenum is prone to intestinal obstruction by narrowed angle between the SMA and the abdominal aorta. Clinical symptoms include postprandial abdominal distension, epigastric pain, nausea, and vomiting. SMA syndrome and nutcracker syndrome have common features that result from narrowed aortomesenteric angle. However, it is very rare for both syndromes to occur simultaneously, so the two syndromes are regarded as separate diseases. This is a report on a case of nutcracker syndrome with SMA syndrome in a child who presented gross hematuria, recurrent abdominal pain and vomiting. To our knowledge, nutcracker syndrome simultaneous with SMA syndrome has not been previously reported in pediatric patient, especially with an exhibition of gross hematuria. This case suggests that the simultaneous presence of SMA syndrome with the same pathogenesis needs to be considered when nutcracker syndrome is suspected in pediatric patients with hematuria.
Nutcracker syndrome is a disease in which left renal vein (LRV) is compressed between the aorta and the superior mesenteric artery (SMA) to cause hematuria [1]. This is caused by a decrease in the aortomesenteric angle, which is the angle between LRV and SMA, due to weight loss, external or intraperitoneal compression, and increased mesenteric tension [2]. If the third part of the duodenum is squeezed due to a reduced aortomesenteric angle, SMA syndrome that causes intestinal obstruction occurs [3]. These two diseases have the same pathogenesis of a decrease in aortomesenteric angle, but the simultaneous occurrence of both diseases is quite rare [4]. This is a report on a case of nutcracker syndrome combined with SMA syndrome in a 14-year-old female child who presented with gross hematuria and recurrent abdominal pain and vomiting.
A 14-year-old female patient visited the outpatient clinic with gross hematuria, recurrent abdominal pain and vomiting. The patient had a past history of recurrent abdominal pain and vomiting for 4 to 5 years, but there was a history of failure to diagnose the cause despite being admitted to other hospitals a total of 5 times. Three years ago, she had undergone a laparoscopic ovarian cystectomy for a hydrosalpinx. However, she still complained of recurrent intermittent abdominal pain, nausea and vomiting about once a week. In addition, gross hematuria brown in color occurred about once every 3ŌĆō4 days one month prior to the clinic visit, and urinalysis showed occult blood 2+ on school health examination. There was no significant family history or social history.
The patient was very underweight with a height 157 cm (25ŌĆō50 percentile), body weight 37 kg (<3 percentile), and a body mass index (BMI) of 15.01 kg/m2 (<3 percentile). The signs of vitality were 111/74 mmHg in blood pressure, pulse rate of 88 beats/min, respiratory rate of 22 breaths/min and body temperature of 36.8Ōäā. The mental state of the child was clear, and physical examination showed mild upper abdominal tenderness.
Gross urine color was brown and there were no blood clots in the urine. On urine tests, urinary occult blood 3+ was observed. Microscopic findings showed more than 100 red blood cells/HPF, no erythrocyte cast, and dysmorphic RBC less than 30% and myoglobin (-), respectively. The urine protein/creatinine ratio was increased to 0.48 at the first spot urine test in the morning, but it was normalized to 0.16 on the 2nd day of hospitalization, and the urine calcium/creatinine ratio was normal at 0.10. Urine mycobacterial cultures were negative.
Laboratory test results were all in the normal range. Complete blood count was leukocyte of 6,500/╬╝L, hemoglobin of 11.8 g/dL, platelet count of 280,000/╬╝L. A blood chemistry test revealed serum C-reactive protein of 0.01 mg/dL, total protein 5.7 g/dL, albumin 3.6 g/dL, aspartate aminotransferase 17 IU/L, alanine aminotransferase 8 IU/L, total bilirubin 0.4 mg/dL, blood urea nitrogen 9 mg/dL, creatinine 0.6 mg/dL, sodium 140 mEq/L, potassium 4.5 mEq/L, and chlorine 108 mEq/L, and in the general blood test, prothrombin time 13.1 sec and activated partial thromboplastin time 32.9 sec. According to the Schwartz estimate, the glomerular filtration rate was normal at 143.9 ml/min/1.73m2. An immune serum test showed complement 3 83.5 mg/dL, complement 4 12.8 mg/dL, immunoglobulin A 246.93 mg/dL, antistreptolysin O 276.90 IU/mL and hepatitis B surface antigen (-), hepatitis B surface antibody (-), rheumatoid factor 9.80 IU/mL , antinuclear antibody (-).
On the plain abdominal X-ray, an extended stomach was observed while standing, and the air-fluid level was seen across the second portion of the duodenum. Doppler ultrasonography (USG) revealed that LRV that runs between the aorta and the SMA is very narrow (aortomesenteric distance: 5 mm), and the anterior-posterior (AP) diameter ratio in the aortomesenteric area (the hilar to the aortomesenteric portion=0.69 cm/0.13 cm) was 5.3, and the ratio of LRV peak velocity (aortomesenteric portion to the hilar=95 cm/sec / 18 cm/sec) was 5.27 and the artomesenteric angle was 18┬░ (Fig. 1). These findings were consistent with nutcracker syndrome. No specific findings in the size, shape, and echogenicity of bilateral kidneys were found. Abdomen & pelvis computed tomography (CT) (enhancement) showed a compressed LRV between aorta and SMA, the aorto-SMA distance was 4.6 mm, and the aorto-mesenteric angle was 18┬░. This is a finding probable of nutcracker syndrome. At the level of the duodenum, the duodenal third portion was compressed and the stomach was bulging along with the first and second portions of the duodenum. The aorto-SMA distance was 5.4 mm and the aortomesenteric angle was 18┬░. This is an indicative finding for SMA syndrome (Fig. 2). Upper gastrointestinal (UGI) series showed mild distention of the proximal duodenum (1st and 2nd part) and hesitancy of the contrast flow from the 3rd to 4th part of the duodenum in a supine position. This suggests SMA syndrome (Fig 3). We diagnosed this patient as having simultaneous nutcracker syndrome and SMA syndrome.
Doppler USG and contrast-enhanced CT showed characteristic features of SMA syndrome and nutcracker syndrome. This may be due to the child's unfavorable eating habits and a very skinny body with low body weight (BMI <3 percentile), or to the structural change that affects the angle between the aorta and the superior mesenteric artery after laparoscopic ovarian cystectomy performed three years prior [3]. The patient's vital signs were stable, and there was no serious complication of SMA syndrome such as gastrointestinal perforation, or hematologic findings of nutcracker syndrome accompanying anemia which requires surgical intervention [1]. Conservative nonsurgical treatment methods were recommended after consulting with the department of pediatric surgery. In addition, the patient's position was maintained in the left lateral deviation position, prone position, or knee-chest posture, resulting in improvement of the intestinal obstruction due to SMA syndrome [3]. On the 2nd day of admission, gross hematuria improved. No microscopic hematuria was seen on the 11th day after admission. Nausea, vomiting, and abdominal pain improved on the fourth day of admission. No vomiting was observed on the sixth day of admission, and symptoms such as abdominal pain were mild. On the 8th day of admission, the child was discharged from the hospital and her weight had increased by 1kg compared with that at admission. The patient was followed up with at the outpatient clinic with no visible gross hematuria, abdominal pain, or nausea and vomiting.
This is a case report of recurrent abdominal pain and vomiting for which a cause had not been found for several years. We diagnosed the child with nutcracker syndrome and SMA syndrome through differential diagnosis of gross hematuria. It is significant that the symptoms were improved by conservative treatment of these rarely combined two diseases.
Nutcracker syndrome is defined as a case in which the LRV is compressed by the aorta and the SMA and accompanied by gross or microscopic hematuria, orthostatic proteinuria, abdominal pain, flank pain, pelvic congestion in females, and varicoceles in males. Until now, the pathophysiology of nutcracker syndrome has not been completely determined. However, up to now, it has been reported that the LRV is pulled just below the aorta due to fat reduction around the kidney, posterior displacement of the kidney, and abnormal branch arteries from the superior mesenteric artery [5]. In this case, it is thought that the posterior dislocation of the left kidney was caused by a decrease in the fat around the kidney due to the low body weight and deformation of the structure affecting the aortomesenteric angle after surgery. Left renal angiography is the most accurate diagnostic method, but this invasive test can cause complications such as dyspnea and hypotension. We used CT and Doppler USG, which are the most commonly used noninvasive methods. According to Kim et al. [5], the CT diagnostic criteria for nutcracker syndrome are narrowing (beak sign) of the LRV in the aortomesenteric part, and the ratio of the LRV diameter (hilar to aortomesenteric) is more than 4.9 and the aortomesenteric angle is less than 41┬░ with collateral venous circulation. The USG diagnostic criteria for nutcracker syndrome [5] is that the AP diameter ratio (the hilar to the aortomesenteric portion) in the aortomesenteric area is 5.0 or more, or the ratio of LRV peak velocity (aortomesenteric portion to the hilar) is 5.0 or more. This case showed a decrease in the fat around the kidney and the compression of the renal vein on the CT and Doppler USG, which meets the above criteria and could be diagnosed as nutcracker syndrome with gross hematuria, microscopic hematuria, and abdominal pain. Treatment depends on the severity of the symptoms and hematuria and flank pain without anemia can be observed without any special treatment. In particular, hematuria improves in 75% of patients with nutcracker syndrome within 2 years under 18 years of age [6]. Anemia due to persistent gross hematuria, severe abdominal pain, or failure to perform conservative treatment should require intervention such as nephropexy or LRV stent insertion. In this case, there was no indication of surgical procedure. Therefore, conservative treatment was attempted first, and both gross and microscopic hematuria were improved.
In this case, nutcraker syndrome and SMA syndrome were diagnosed simultaneously. SMA syndrome is a disease in which the lumen is compressed by the aortomesenteric angle narrowed to the third part of the duodenum and the male to female ratio is 1:1.58ŌĆō3, which is relatively co mmon in women in their 30ŌĆō40s [7]. The causes of this disease are largely classified into three categories: 1) weight loss, 2) external or intraperitoneal pressure, and 3) increased mesenteric tension [3]. SMA syndrome commonly occurs in people who are underweight, but other factors are involved in clinical symptoms [8]. It has been reported that rapid weight loss and other changes in metabolic status result in a decrease in the adipose tissue of the mesentery and posterior abdominal cavity, resulting in a decrease in the aortomesenteric angle and causing SMA syndrome [9]. SMA syndrome can be induced by abdominal casting, external abdominal compression, or intraperitoneal compression by a tumor or abdominal aortic aneurysm [10,11]. Increased mesenteric tension due to structural deformations affecting the aortomesenteric angle caused by surgery is also a risk factor [3]. Clinical symptoms include epigastric pain, continuous nausea, and vomiting. Left lateral deviation, prone, or knee-chest postures may widen the aortomesenteric angle and decrease mesenteric tension, which may improve symptoms. The aortomesenteric distance and the aortomesenteric angle are measured using CT, and the normal range is 10 to 28 mm and 25 to 60┬░, respectively. In this case, the aorto-SMA distance was 5.4 mm and the aortomesenteric angle was 18┬░, which was acceptable for the diagnosis of SMA syndrome. Most cases are often improved with conservative treatment. Surgical treatment is limited to failure of conservative treatment. Conservative treatments include decompression through nasogastric drainage and electrolyte correction, intravenous hypertrophic fluid therapy, and nutrition through a nasojejunal tube. It can cause an increase in fat and body weight around the kidneys. In this case, weight gain was 1 kg before discharge due to treatment of active fluid supply, dietary habit correction, nutritional support, and restricting activities. Both symptoms of nutcracker syndrome and SMA syndrome were improved. In addition, we searched the previous case reports on SMA syndrome combined with nutcracker syndrome. The summary of case reports is described in Table 1.
SMA syndrome and nutcracker syndrome have common features that result from narrowed aortomesenteric angle. However, it is very rare for both syndromes to occur simultaneously, so the two syndromes are regarded as separate diseases. To our knowledge, nutcracker syndrome simultaneous with SMA syndrome has not been previously reported in pediatric patient, especially with an exhibition of gross hematuria. This case suggests that the simultaneous presence of SMA syndrome with the same pathogenesis needs to be considered when nutcracker syndrome is suspected in children with hematuria.
References
1. Kim JM, Choi YJ, Lee JS. Spontaneous resolution of childhood nutcracker syndrome. Child Kidney Dis 2006;10:213-18.
2. Myung Jin Oh. Superior mesenteric artery syndrome combined with renal nutcracker syndrome in a young male: A Case Report. Korea J Gastroenterol 2017;70:253-60.

3. Kim EB, Lee TH. Superior mesenteric artery syndrome: past and present. Korean J Med 2013;84:28-36.

4. Zaraket V, Deeb L. Wilkie's syndrome or superior mesenteric artery syndrome: fact or fantasy? Case Rep. Gastroenterol 2015;9:194-9.
5. Kim SH, Heo JU, Tang YK, Kim JH, Shu YC, Ki Tai Kim, et al. Superior mesenteric artery syndrome with nutcracker syndrome in a patient with type 1 diabetes mellitus. Korean J Med 2012;83:613-8.

6. Shin JI, Park JM, Lee SM, Shin YH, Kim JH, Lee JS, et al. Factors affecting spontaneous resolution of hematuria in childhood nutcracker syndrome. Pediatr Nephrol 2005;20:609-13.


7. Akin JT Jr, Gray SW, Skandalakis JE. Vascular compression of the duodenum: presentation of ten cases and review of the literature. Surgery 1976;79:515-22.

9. Froese AP, Szmuilowicz J, Bailey JD. The superior-mesentericartery syndrome: cause or complication of anorexia nervosa? Can Psychiatr Assoc J 1978;23:325-7.


10. Anderson JR, Earnshaw PM, Fraser GM. Extrinsic compression of the third part of the duodenum. Clin Radiol 1982;33:75-81.


11. Edwards KC, Katzen BT. Superior mesenteric artery syndrome due to large dissecting abdominal aortic aneurysm. Am J Gastroenterol 1984;79:72-4.

12. Pivawer G, Haller JO, Rabinowitz SS, Zimmerman DL. Superiormesenteric artery syndrome and its ramifications. CMIG Extra: Cases 2004;28:8-10.

13. Barsoum MK, Shepherd RF, Welch TJ. Patient with both wilkie syndrome and nutcracker syndrome. Vasc Med 2008;13:247-50.


14. Vulliamy P, Hariharan V, Gutmann J, Mukherjee D. Superior mesenteric artery syndrome and the 'nutcracker phenomenon'. BMJ Case Rep 2013;2013:pii: bcr2013008734.

15. Inal M, Unal Daphan B, Karadeniz Bilgili MY. Superior mesenteric artery syndrome accompanying with nutcracker syndrome: a case report. Iran Red Crescent Med J 2014;16:e14755.



Fig.┬Ā1.
Images of Doppler USG. (A) The diameters of LRV in the aortomesenteric portion (0.13 cm) and the hilar portion (0.69 cm). (B) The peak velocities in the aortomesenteric portion (95 cm/sec). (C) The peak velocities in the hilar portion (18 cm/sec). (D) The aortomesenteric angle (18┬░).
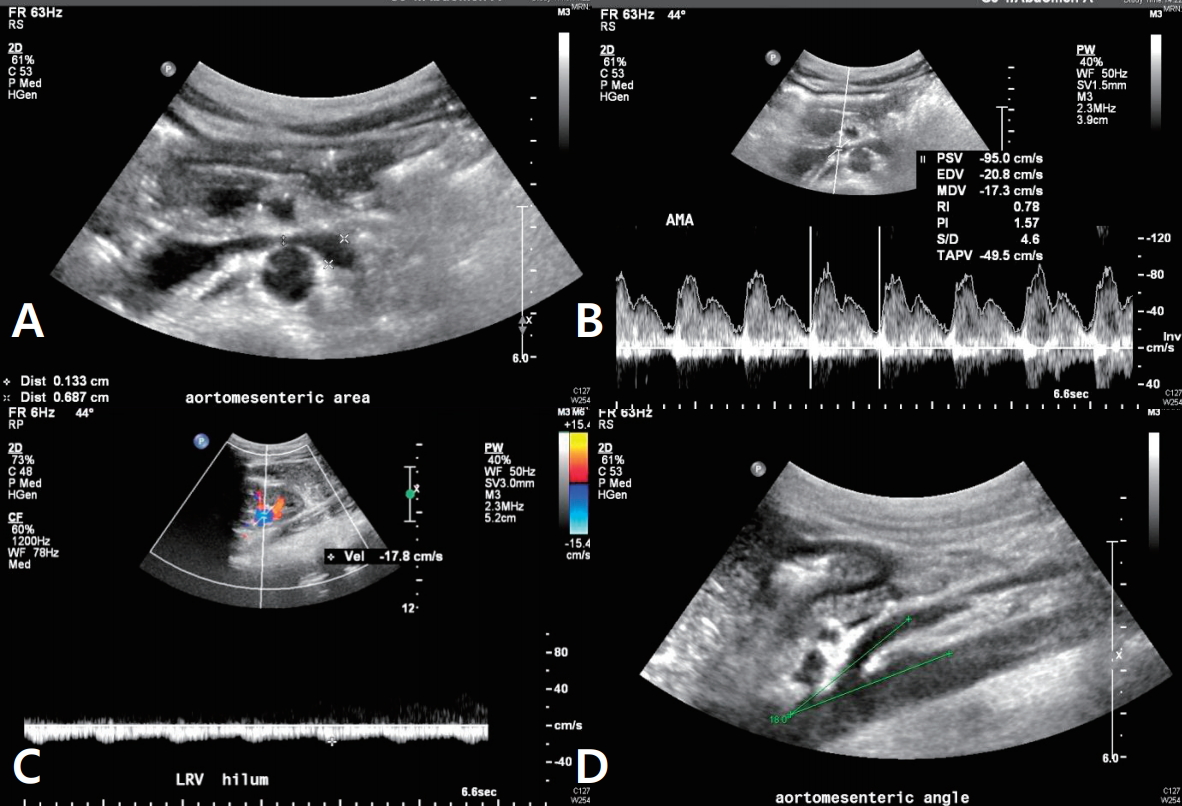
Fig.┬Ā2.
Abdomen & pelvis CT (enhancement). (A) LRV was compressed by the aorta and the superior mesenteric artery (aorto-SMA distance: 4.6 mm). (B) Duodenal 3rd portion was trapped by the decreased aortomesenteric angle in the transverse plane (aorto-SMA distance: 5.4 mm). (C) Aortomesenteric angle was 18 ┬░ in the sagittal plane.
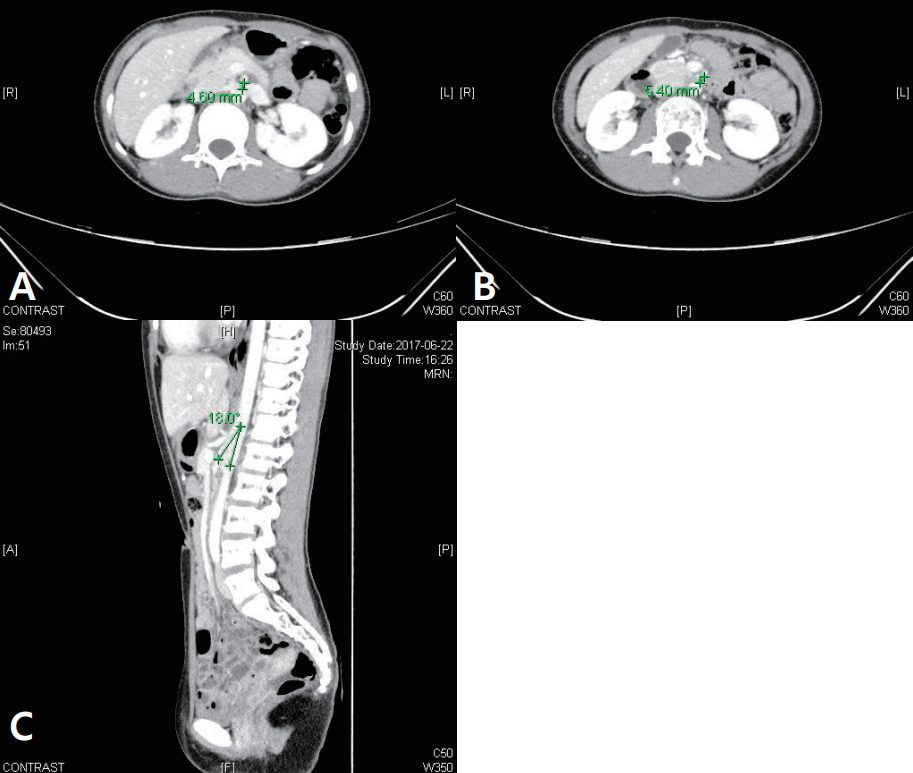
Fig.┬Ā3.
UGI series. An image showed that mild distention of the proximal duodenum (1st and 2nd part) and hesitancy of the contrast flow from the 3rd to 4th part of the duodenum in the supine position.

Table┬Ā1.
Case Reports on SMA Syndrome Combined with Nutcracker Syndrome
| Case | Year | Sex/Age | Chief complaint | Causes | Duration of symptoms | BMI (kg/m2) | Diagnostic methods | Presence of hematuria | Treatments | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Pivawer et al. [12] | 2004 | M/15 | Abdominal pain, vomiting | None | N.A. | N.A. | AXR, APCT, UGI | N.A. | Nasogastric decompression, TPN, hydration | Resolved |
| Barsoum et al. [13] | 2008 | F/29 | Vomiting, epigastric pain | Surgery due to brain stem ganglioma | 3 years | 14 | APCT, UGI, EGD | No | Enteral nutritional support with jejunostomy feeding tube | Resolved |
| Kim et al. [5] | 2012 | M/24 | Vomiting, left flank pain | Insulin treatment discontinued | 3 weeks | 17 | AXR, APCT | Yes | Nasogastric decompression, TPN, insulin treatment | Resolved |
| Vulliamy et al. [14] | 2013 | M/55 | Vomiting, epigastric pain, bloating | Diet | 1 year | 17 | APCT | No | N.A. | N.A. |
| Inal et al. [15] | 2014 | M/28 | Vomiting, epigastric pain, bloating | None | 3ŌĆō4 years | N.A. | APCT | No | TPN, jejunostomy feeding tube | Resolved |
| Nunn et al. [16] | 2015 | F/19 | Epigastric pain, vomiting, anorexia | None | 3 years | N.A. | APCT | No | Nasogastric decompression, TPN, stocking, LMWH | Resolved |
| Iqbal et al. [17] | 2016 | M/62 | None | Rectal carcinoma | N.A. | N.A. | APCT | N.A. | Conservative treatments | N.A. |
| Oh MJ. [2] | 2017 | M/23 | Vomiting, nausea, bloating | Physical exhaustion | 1 year | 21 | AXR, APCT, UGI, EGD, USG | No | Laparoscopic duodenojejunostomy | Resolved |
| This case | 2017 | F/14 | Abdominal pain, vomiting, nausea, gross hematuria | Diet | 4ŌĆō5 years | 15 | AXR, APCT, UGI, USG | Yes | Conservative treatments, hydration | Resolved |
Abbreviations: M, male; F, female; N.A., not available; BMI, body mass index; AXR, abdominal X-ray; APCT, abdomen & pelvis computed tomography; UGI, upper gastrointestinal series; EGD, esophagogastroduodenoscopy; USG, ultrasonography; TPN, total parentral nutrition; LMWH, low molecular weight heparin.
- TOOLS
-
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link XML Download
XML Download Full text via DOI
Full text via DOI-
 Download Citation
Download Citation
- Download Citation
-
- Close
 Print
Print-
Share :



-
METRICS

-
- 3 Crossref
- 0 Scopus
- 12,232 View
- 186 Download
- Related articles
-
Nutcracker syndrome combined with immunoglobulin A nephropathy: two case reports2023 December;27(2)